Rheumatoid arthritis (RA) is an autoimmune disease that results in a chronic, systemic inflammatory disorder that may affect many tissues and organs, but principally attacks flexible (synovial) joints. It can be a disabling and painful condition, which can lead to substantial loss of functioning and mobility if not adequately treated. The hallmark feature of this condition is persistent symmetric polyarthritis (synovitis) that affects the hands and feet, though any joint lined by a synovial membrane may be involved. Extra-articular involvement of organs such as the skin, heart, blood vessels, lungs, and eyes can be significant. Although rheumatoid arthritis affects approximately 1% of the world population. It can occur at any age and usually begins after age 40 (Peak incidence is between the 4th and 6th decade). The disorder is much more common in women than in men. Genetic and autoimmune factors are mainly responsible for the initiation of the disease process.
Juvenile Rheumatoid Arthritis (JRA)
Juvenile rheumatoid arthritis causes joint inflammation and stiffness for more than six weeks in a child aged 16 or younger. Even though infectious agents such as viruses, bacteria, and fungi have long been suspected, the cause of rheumatoid arthritis is unknown. Treatment focuses on controlling symptoms and preventing joint damage.
Table of Contents
Epidemiology
Worldwide, the annual incidence of RA is approximately 3 cases per 10,000 populations, and the prevalence rate is approximately 1%, increasing with age and peaking between the ages of 35 and 50 years. In 2010, it resulted in about 49,000 deaths globally.
About 1.5 million people in the United State have RA. Nearly three times as many women have the disease as men. In women, RA most commonly begins between ages 30 and 60. In men, it often occurs later in life.
RA is a chronic disease, and although rarely, a spontaneous remission may occur. The natural course is almost invariably one of the persistent symptoms, waxing and waning in intensity, and progressive deterioration of joint structures leading to deformations and disability.
Etiology
The cause of RA is unknown. Genetic, environmental, hormonal, immunologic, and infectious factors may play significant roles. Socioeconomic, psychological, and lifestyle factors (e.g., tobacco use, the main environmental risk) may influence disease outcome.
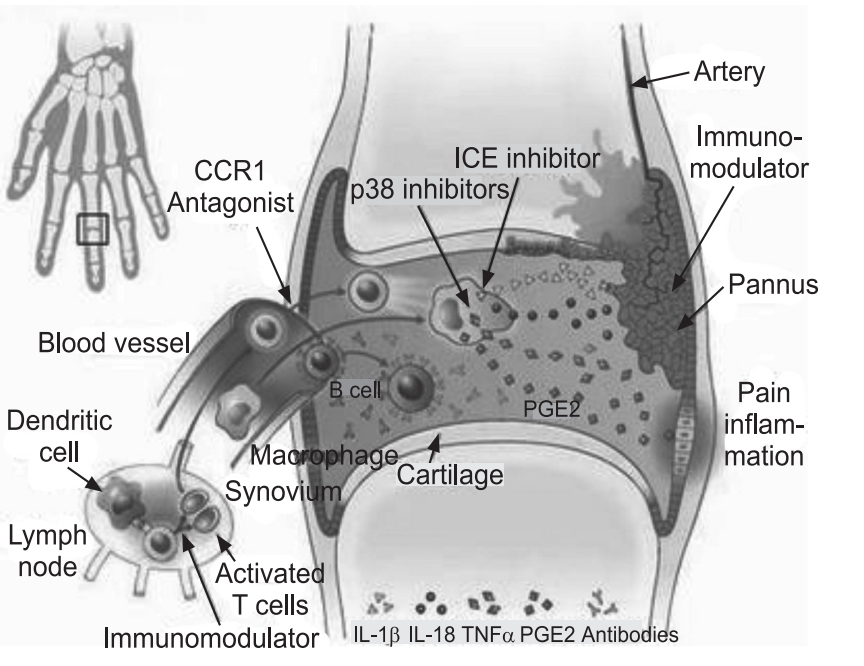
Immunologic factors: Rheumatoid arthritis occurs when the immune system attacks the synovium, the lining of the membranes that surround joints. All of the major immunologic elements play fundamental roles in the initiation, propagation, and maintenance of the autoimmune process of RA. The exact orchestration of the cellular and cytokine events that lead to pathologic consequences, such as synovial proliferation and subsequent joint destruction is complex. It involves T and B lymphocytes, antigen-presenting cells (e.g., B cells, macrophages, dendritic cells), and numerous cytokines. Aberrant production and regulation of both pro-inflammatory and anti-inflammatory cytokines and cytokine pathways are found in RA. The resulting inflammation thickens the synovium, which can eventually destroy the cartilage and bone within the joint. The tendons and ligaments that hold the joint together weaken and stretch. Gradually, the joint loses its shape and alignment.
Genetic factors: Half of the risk for RA is believed to be genetic. It is strongly associated with the inherited tissue type major histocompatibility complex (MHC) antigen HLA-DR4 (most specifically DR0401 and 0404), and the genes PTPN 22 and PAD I4, hence family history is an important risk factor. Inheriting the PTPN22 gene has been shown to double a person’s susceptibility to RA. PADI4 has been identified as a major risk factor in people of Asian descent, but not in those of European descent. The first-degree relatives’ prevalence rate is 2–3% and disease genetic concordance in monozygotic twins is approximately 15–20%.
Infectious agents: For many decades, numerous infectious agents have been suggested as potential causes of RA, including Mycoplasma organisms, Epstein-Barr virus (EBV), and rubella virus.
Hormonal factors: Sex hormones may play a role in RA, as evidenced by the disproportionate number of females with this disease, its amelioration during pregnancy, its recurrence in the early postpartum period, and its reduced incidence in women using oral contraceptives. Hyperprolactinemia may be a risk factor for RA.
Other factors: Smoking is the most significant non-genetic risk with RA being up to three times more common in smokers than non-smokers, particularly in men. Vitamin D deficiency is more common in patients with rheumatoid arthritis than in the general population. However, whether vitamin D deficiency is a cause or a consequence of the disease remains unclear.
Pathophysiology
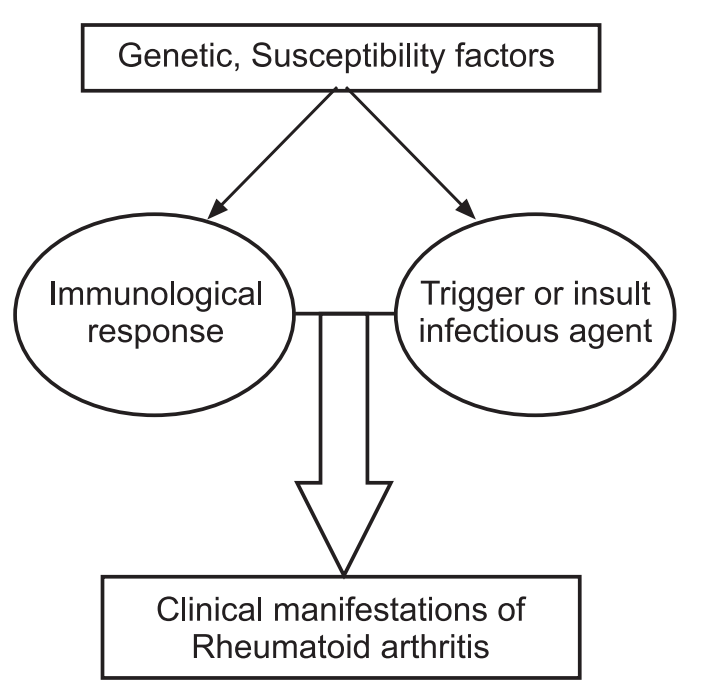
The pathogenesis of RA is not completely understood. An external trigger (e.g., cigarette smoking, infection, or trauma) that triggers an autoimmune reaction, leading to synovial hypertrophy and chronic joint inflammation along with the potential for extra-articular manifestations, is theorized to occur in genetically susceptible individuals.
Synovial cell hyperplasia and endothelial cell activation are early events in the pathologic process that progresses to uncontrolled inflammation and consequent cartilage and bone destruction. Genetic factors and immune system abnormalities contribute to disease propagation.
CD4 T cells, mononuclear phagocytes, fibroblasts, osteoclasts, and neutrophils play major cellular roles in the pathophysiology of RA, whereas B cells produce autoantibodies (Rheumatoid factors). Abnormal production of numerous cytokines, chemokines, and other inflammatory mediators (e.g., tumor necrosis factor-alpha [TNF-α], interleukin [IL1, IL-6, IL-8], transforming growth factor-beta [TGF-β], fibroblast growth factor [FGF], and platelet-derived growth factor [PDGF]) has been demonstrated in patients with RA.
Ultimately, inflammation and exuberant proliferation of the synovium (pannus) lead to the destruction of various tissues, including cartilage, bone, tendons, ligaments, and blood vessels. Although the articular structures are the primary sites involved in RA, other tissues are also affected.
Rheumatoid Arthritis and Joint Inflammation:
Joint inflammation is a hallmark of rheumatoid arthritis. That includes:
Stiffness: The joint is harder to use and might have a limited range of motion. “Morning stiffness” is one of the hallmark symptoms of rheumatoid arthritis. While many people with other forms of arthritis have stiff joints in the morning. People with rheumatoid arthritis take more than an hour (sometimes several hours) before their joints feel loose.
Swelling: Fluid enters the joint and it becomes puffy; this also contributes to stiffness. Pain: Inflammation inside a joint makes it sensitive and tender. Prolonged inflammation causes damage that also contributes to pain.
Redness and warmth: The joints may be somewhat warmer and more pink or red than neighboring skin. Other symptoms: RA can affect many areas of the body. These effects all result from the general process of inflammation, leading to a wide variety of symptoms of rheumatoid arthritis:
- Fatigue,
- Malaise,
- Loss of appetite, which can lead to weight loss,
- Muscle aches.
These feelings have been compared to having the flu, although they are usually less intense and longer-lasting. Rheumatoid arthritis may affect other areas of the body. Involvement of multiple areas of the body occurs and is more common with moderate to severe rheumatoid arthritis.
Complications
Rheumatoid Arthritis Skin Problems: Rheumatoid arthritis (RA) is primarily a disease of the joints. But the disease and many of the medications used to treat it can also affect the skin, causing problems as diverse as sun sensitivity, rash, and firm lumps of tissue called nodules.
Lung involvement, due to either damage to the lungs or inflammation of the lining around the lungs, is common but sometimes causes no symptoms. If shortness of breath develops, it can be treated with drugs that reduce inflammation in the lungs.
Rheumatoid arthritis can even affect a joint in the voice box or larynx (cricoarytenoid joint), causing hoarseness.
Rheumatoid arthritis can cause inflammation in the lining around the heart, but it usually has no symptoms. If symptoms do develop, it may cause shortness of breath or chest pain. In addition, people with rheumatoid arthritis are more likely to develop clogged arteries in their hearts, which can lead to chest pain and heart attacks.
The eyes are affected in less than 5% of people with rheumatoid arthritis. When the eyes are affected, symptoms can include red, painful eyes, or possibly dry eyes.
Early rheumatoid arthritis tends to affect smaller joints first, particularly the joints that attach fingers to hands and toes to feet. As the disease progresses, symptoms often spread to the knees, ankles, elbows, hips, and shoulders. In most cases, symptoms occur in the same joints on both sides of the body.
Tests and Diagnosis
Rheumatoid arthritis can be difficult to diagnose in its early stages because the early signs and symptoms mimic those of many other diseases. There is no one blood test or physical finding to confirm the diagnosis.
Physical exam: To check joints for swelling, redness, warmth, and also check reflexes and muscle strength.
Laboratory studies: Routine viral screening by serologic testing neither significantly facilitate the diagnosis of RA in patients with early RA, nor it is helpful as a potential identifier of disease progression.
Potentially useful laboratory studies in suspected RA fall into 3 categories: markers of inflammation, hematologic parameters, and immunologic parameters and include the following:
- Erythrocyte sedimentation rate (ESR)
- C-reactive protein (CRP) level
- Complete blood count (CBC)
- Rheumatoid factor (RF) assay
- Antinuclear antibody (ANA) assay
Markers of inflammation: The ESR and the CRP level are associated with disease activity.
Hematologic parameters: People with rheumatoid arthritis tend to have an elevated erythrocyte sedimentation rate (ESR), which indicates the presence of an inflammatory process in the body. C-reactive protein (CRP) levels are an even better indication than ESR of the amount of inflammation present. In people with rheumatoid arthritis, if the CRP is high, it suggests that there is significant inflammation or injury in the body.
Both CRP and ESR levels are used to monitor disease activity and to monitor how well someone is responding to treatment. The CBC commonly demonstrates anemia of chronic disease and correlates with disease activity; it improves with successful therapy. Hypochromic anemia suggests blood loss, commonly from the gastrointestinal (GI) tract (associated with the use of nonsteroidal anti-inflammatory drugs). Anemia may also be related to disease-modifying antirheumatic drug (DMARD) therapy.
Thrombocytosis is common and also associated with disease activity. Thrombocytopenia may be a rare adverse event of therapy and may occur in patients with Felty syndrome. Leukocytosis may occur but is usually mild. Leukopenia may be a consequence of therapy or a component of Felty syndrome, which may then respond to DMARD therapy.
Immunologic parameters: Abnormal antibodies can be found in the blood of people with rheumatoid arthritis with simple blood testing. An antibody “rheumatoid factor” (RF) can be found in 80% of patients with rheumatoid arthritis. Patients who are felt to have rheumatoid arthritis and do not have positive rheumatoid factor testing are referred to as having “seronegative rheumatoid arthritis”. Citrulline antibody (also referred to as anticitrullinated antibody, anti-cyclic citrullinated peptide antibody, and anti-CCP antibody) is present in 50%-75% of people with rheumatoid arthritis. It is useful in the diagnosis of rheumatoid arthritis when evaluating cases of unexplained joint inflammation. A test for citrulline antibodies is especially helpful in looking for the cause of previously undiagnosed inflammatory arthritis when the traditional blood test for rheumatoid arthritis, rheumatoid factor, is not present. Citrulline antibodies have been felt to represent the earlier stages of rheumatoid arthritis in this setting. Citrulline antibodies also have been associated with more aggressive forms of rheumatoid arthritis. Another antibody called the “antinuclear antibody” (ANA) is also frequently found in people with rheumatoid arthritis.
X-rays: X-rays of the hands and feet are generally performed in people with polyarthritis. It may be applicable to help track the progression of rheumatoid arthritis in joints over time.
Other medical imaging techniques such as magnetic resonance imaging (MRI) and ultrasound are also used in RA.
Treatments and Drugs
There is no cure for rheumatoid arthritis. Medications can reduce inflammation in joints in order to relieve pain and prevent or slow joint damage. Occupational and physical therapy helps how to protect joints. If joints are severely damaged by rheumatoid arthritis, surgery may be necessary.
Medications: Many drugs used to treat rheumatoid arthritis have potentially serious side effects.
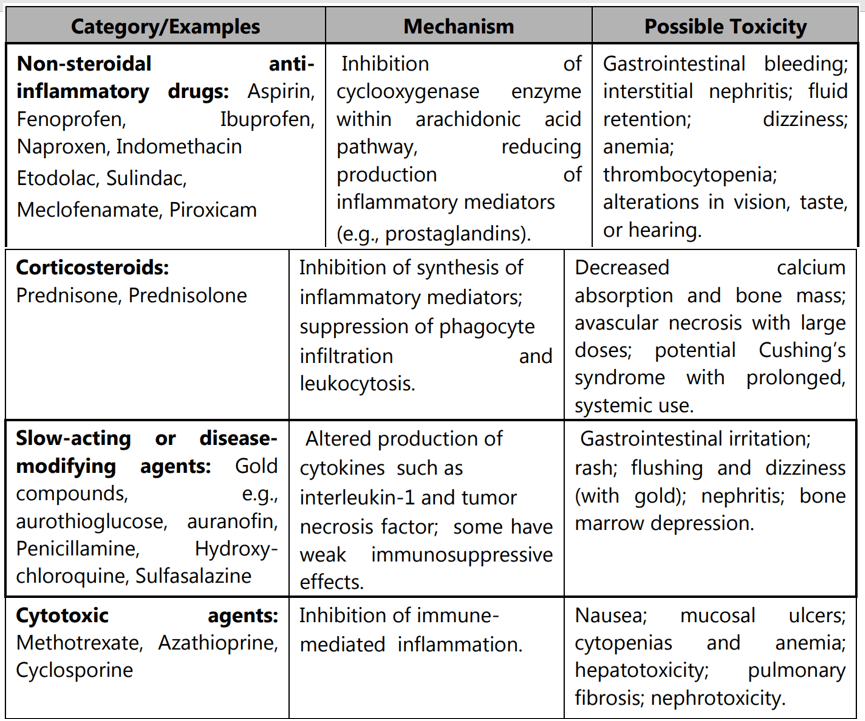
NSAIDs: NSAIDs can relieve pain and reduce inflammation. (e.g. Aspirin, Fenoprofen, Piroxicam, Indomethacin, etc.)
Steroids: Corticosteroid medications, such as prednisone, reduce inflammation and pain and slow joint damage. Side effects may include thinning of bones, cataracts, weight gain, and diabetes. Corticosteroids are used to relieve acute symptoms, with the goal of gradually tapering off the medication.
Disease-modifying antirheumatic drugs (DMARDs): These drugs can slow the progression of rheumatoid arthritis and save the joints and other tissues from permanent damage. Common DMARDs include Gold, d-penicillamine, chloroquine or hydroxychloroquine, sulfasalazine, leflunomide, etc. Side effects vary but may include liver damage, bone marrow suppression, and severe lung infections.
Immunosuppressants: These medications act to suppress the immune system, which is out of control in rheumatoid arthritis. Examples include cyclosporine, azathioprine, and methotrexate. These medications can increase susceptibility to infection.
TNF-inhibitors: Tumor necrosis factor-alpha (TNF-α) is an inflammatory substance produced by the body. TNF-inhibitors can help to reduce pain, morning stiffness, and tender or swollen joints. Examples include etanercept, infliximab, adalimumab, golimumab, and certolizumab. Potential side effects include nausea, diarrhea, hair loss, and an increased risk of serious infections.
Other drugs: Several other rheumatoid arthritis drugs target a variety of processes involved with inflammation in the body. These drugs include anakinra, abatacept, rituximab, tocilizumab, and tofacitinib. Side effects vary but may include itching, abdominal pain, headache, runny nose, or sore throat.
Surgery: If medications fail to prevent or slow joint damage, surgery requires repairing damaged joints. Surgery may help restore the ability to use joints. It can also reduce pain and correct deformities. Rheumatoid arthritis surgery may involve one or more of the following procedures:
- Total joint replacement
- Tendon repair
- Joint fusion
Make sure you also check our other amazing Article on: Alcoholic liver Disease
