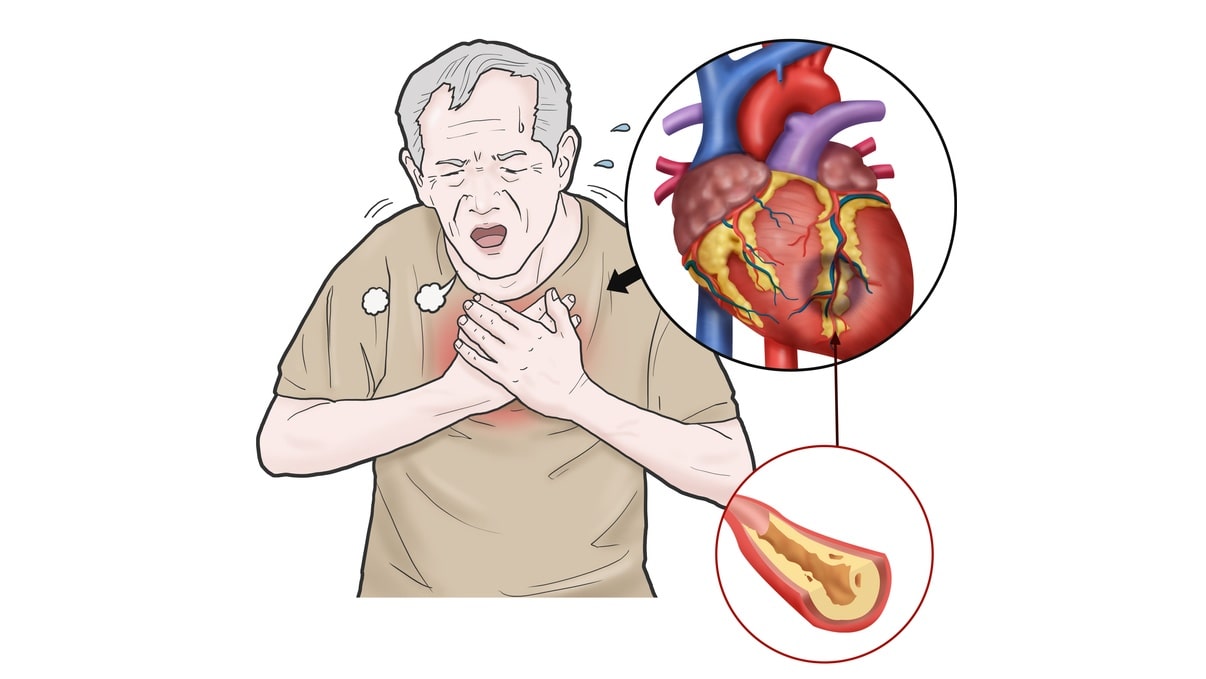
Angina pectoris is a clinical syndrome of Ischemic heart disease (IHD) resulting from transient myocardial ischemia if the heart muscle does not get as much blood as it needs. This usually happens because one or more of the heart’s arteries is narrowed or blocked. It is characterized by paroxysmal pain in the substernal or precordial region of the chest which is aggravated by an increase in the demand of the heart and relived by a decrease in the work of hearing. Often, the pain radiates to the left arm, neck jaw, or right arm.
There are thee overlapping clinical patterns of angina pectoris with some differences in their pathogenesis:
Table of Contents
Types of Angina Pectoris
Stable or Typical Angina:
It can also be referred to as exertional angina. It is associated with severe narrowing of the coronary artery due to the build-up of plaque (plaque is excess cholesterol and other debris that has built up inside a coronary artery). With exertion, like walking up a hill or climbing stairs, the heart works harder and needs more oxygen. If it can not get enough oxygen, a person develops symptoms of Angina, the condition improves with rest. During the attacks, there is depression of ST-segment in the ECG due to poor perfusion of the subendocardial region of the left ventricle. But there is no elevation of enzymes in the blood as there is no irreversible myocardial injury.
Unstable Angina:
Unstable angina occurs when the narrowing of the coronary artery due to the build-up of plaque becomes so severe that not enough blood gets through to keep the heart functioning normally, even at rest. In most patients, it is induced by acute plaque change with superimposed partial thrombosis, distal embolization of the thrombus, and/or vasospasm. The morphologic changes in the heart are essentially those of coronary atherosclerosis and its associated lesions. In unstable angina, lack of oxygen to the heart leads to necrosis of heart tissue. Thus, increasing the chances of myocardial infarction requires emergency treatment. The distinction between unstable angina and acute myocardial infarction is made by ST-segment changes on ECG. In acute MI, ST-segment elevates while unstable angina may have non-ST-segment elevation.
Variant Angina (Vasospastic angina, Prinzmental’s angina.):
Rare type of angina caused basically due to spasm of coronary arteries. Variant angina may occur during resting or active state, presence or absence of clogged arteries from atherosclerosis. Spasms lead to decreased blood flow to the heart and hence increase the risk of a heart attack. ECG shows ST-segment elevation due to transmural ischemia. These patients respond well to vasodilators like nitroglycerin.
Symptoms
- The most prominent symptom of angina is pain or pressure in the chest. It may feel like squeezing or fullness in the middle of the chest and it can radiate outward to the neck, jaw, shoulder, back, or arms.
- With stable angina, episodes of pain are a regular occurrence and become predictable as triggers are identified. It normally lasts less than five minutes and goes away with rest and/or medication.
- With unstable angina, the pain is different from that experienced with stable angina and is not predictable. It is sharper, unexpected (no trigger has been identified), and does not go away with rest or medication.
- Variant angina causes sharp bursts of pain, often in the middle of the night. They can last up to 30 minutes but may respond to medication.
- Other symptoms can include numbness or tingling, anxiety, fainting, dizziness, sweating, shortness of breath, pale skin, irregular heartbeat, nausea, or fatigue.
Treatment
Treatment options include:
- Rest
- Medications (Nitroglycerine, β-blockers, calcium channel blockers),
- Percutaneous transluminal coronary angioplasty (PTCA), or
- Coronary artery bypass graft surgery (CABG).
Make sure you also check our other amazing Article on: Ischaemic heart disease