Osteoarthritis (OA) is the most common form of arthritis, affecting millions of people around the world. It can be thought of as a degenerative disorder arising from the biochemical breakdown of articular (hyaline) cartilage in the synovial joints. However, the current view holds that osteoarthritis involves not only the articular cartilage but also the entire joint organ, including the hands, neck, lower back, knees, and hips.
Table of Contents
Types of osteoarthritis
Primary osteoarthritis: It is mostly related to aging. With aging, the water content of the cartilage increases, and the protein makeup of cartilage degenerates.
Secondary osteoarthritis: Secondary osteoarthritis is caused by another disease or condition. Conditions that can lead to secondary osteoarthritis include obesity, repeated trauma or surgery to the joint structures, abnormal joints at birth (congenital abnormalities), gout, diabetes, and other hormone disorders.
Epidemiology
Globally approximately 250 million people have osteoarthritis of the knee (3.6% of the population). Osteoarthritis affects nearly 27 million people in the United States. It is estimated that 80% of the population have radiographic evidence of osteoarthritis by age 65, although only 60% of those will have symptoms. Osteoarthritis globally causes moderate to severe disability in 43.4 million people.
Causes
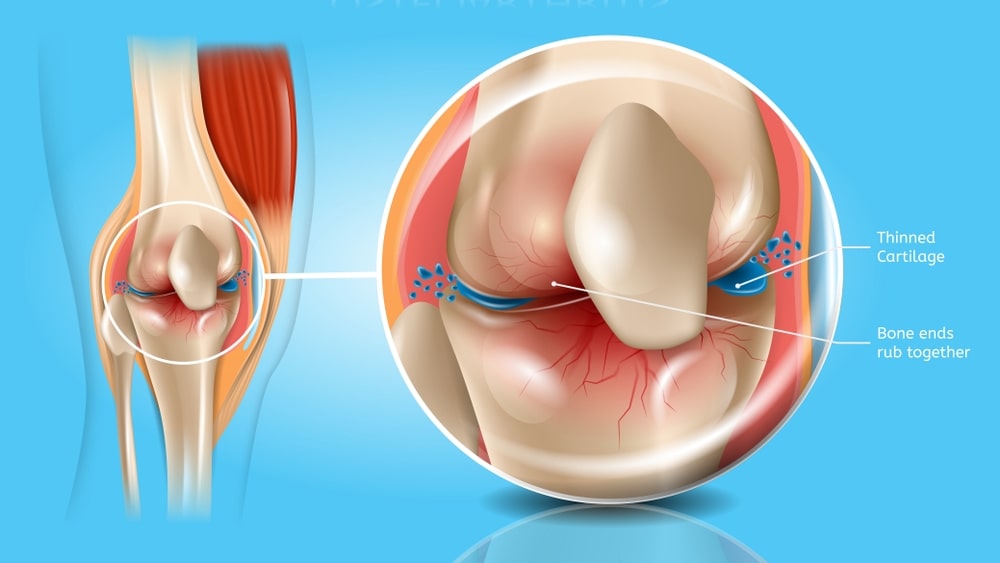
Osteoarthritis occurs when the cartilage that cushions the ends of bones in joints deteriorates over time. Cartilage is a firm, slippery tissue that permits nearly frictionless joint motion. In osteoarthritis, the slick surface of the cartilage becomes rough.
The daily stresses applied to the joints, especially the weight-bearing joints (e.g., ankle, knee, and hip), play an important role in the development of osteoarthritis. Most investigators believe that degenerative or alterations in osteoarthritis primarily begin in the articular cartilage, as a result of either excessive loading of a healthy joint or relatively normal loading of a previously disturbed joint. External forces accelerate the catabolic effects of the chondrocytes and further disrupt the cartilaginous matrix.
Knee osteoarthritis is classified as either primary (idiopathic) or secondary. Among the various structures making up the knee joint, the hyaline joint cartilage is the main target of the harmful influences that cause osteoarthritis and the structure in which the disease begins. About 95% of hyaline cartilage consists of an extracellular matrix.
Older age: The risk of osteoarthritis increases with age.
Sex: Women are more likely to develop osteoarthritis, though the reason is unknown.
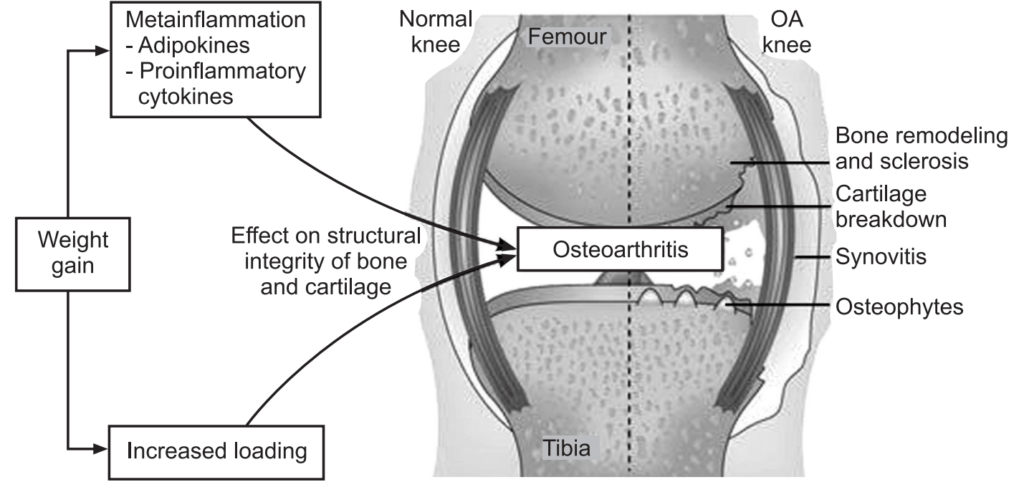
Obesity: Carrying more body weight puts added stress on weight-bearing joints, such as the knees.
Joint injuries: Injuries, such as those that occur when playing sports or from an accident, may increase the risk of osteoarthritis.
- Genetics (significant family history)
- Reduced levels of sex hormones
- Muscle weakness
- Repetitive use (jobs requiring heavy labor and bending)
- Infection
- Crystal deposition
- Acromegaly
- Previous inflammatory arthritis (e.g., burnt-out rheumatoid arthritis)
- Heritable metabolic causes (e.g., alkaptonuria, hemochromatosis, and Wilson disease)
- Hemoglobinopathies (e.g., sickle cell disease and thalassemia)
- Neuropathic disorders leading to a Charcot joint (e.g., syringomyelia, tabesdorsalis, and diabetes)
- Underlying morphologic risk factors (e.g., congenital hip dislocation and slipped femoral capital epiphysis)
- Disorders of bone (e.g., Paget disease and avascular necrosis)
- Previous surgical procedures (e.g., meniscectomy)
Pathophysiology
Osteoarthritis is a degenerative joint disease that may cause gross cartilage loss and morphological damage to other joint tissues, more subtle biochemical changes occur in the earliest stages of osteoarthritis progression. The water content of healthy cartilage is finely balanced by compressive force driving water out and swelling pressure drawing water in. Collagen fibers exert the compressive force, whereas the Gibbs–Donnan effect and cartilage proteoglycans create osmotic pressure which tends to draw water in.
However, during the onset of osteoarthritis, the collagen matrix becomes more disorganized and there is a decrease in proteoglycan content within cartilage. The breakdown of collagen fibers results in a net increase in water content. This increase occurs because there is an overall loss of proteoglycans (and thus a decreased osmotic pull), it is outweighed by a loss of collagen. Without the protective effects of the proteoglycans, the collagen fibers of the cartilage can become susceptible to degradation and thus exacerbate the degeneration. Inflammation of the surrounding joint capsule can also occur, though often mild (compared to rheumatoid arthritis). This can happen, as breakdown products from the cartilage are released into the synovial space, and the cells lining the joint attempt to remove them. New bone outgrowths, called “spurs” or osteophytes, can form on the margins of the joints, possibly in an attempt to improve the congruence of the articular cartilage surfaces. These bone changes, together with the inflammation, can be both painful and debilitating.
Symptoms
Osteoarthritis symptoms often develop slowly and worsen over time. Signs and symptoms of osteoarthritis include:
Pain: Joints may hurt during or after movement. Tenderness: Joint may feel tender if light pressure is applied to it.
Stiffness: Joint stiffness may be most noticeable when waking up in the morning or after a period of inactivity.
Loss of flexibility: The joints are not able to move through their full range of motion.
Grating sensation: You May hear or feel a grating sensation when using the joint.
Bone spurs: These extra bits of bone, which feel like hard lumps, may form around the affected joint.
Physical exam: Physical examination of the affected joint includes, checking for tenderness, swelling, or redness.
Imaging tests: Pictures of the affected joint can be obtained during imaging tests. Examples include:
X-rays: An X-ray may also show bone spurs around a joint. Many people have X-ray evidence of osteoarthritis before they experience any symptoms.
Magnetic resonance imaging (MRI): MRI can be helpful in determining what exactly is causing pain.
Lab tests: Analyzing blood or joint fluid can help to pinpoint the diagnosis.
Blood tests: Blood tests may help to rule out other causes of joint pain, such as rheumatoid arthritis.
Joint fluid analysis: Draw fluid out of the affected joint for inflammation and pain caused by gout or an infection.
Treatments and Drugs
There is no known cure for osteoarthritis, but treatments can help to reduce pain and maintain joint movement.
Medications: Osteoarthritis symptoms can be relieved by a variety of medications, including:
Acetaminophen: Acetaminophen can relieve pain, but it does not reduce inflammation.
NSAIDs: NSAIDs may reduce inflammation and relieve pain. NSAIDs include Ibuprofen, Indomethacin, Diclofenac sodium, Aceclofenac and Naproxen.
Narcotics: Narcotics like codeine may provide relief from more severe osteoarthritis pain.
Lifestyle and home remedies: Lifestyle changes and home treatments also can help to reduce osteoarthritis symptoms.
Rest: Experiencing pain or inflammation in the joint, rest it for 12 to 24 hours.
Exercise: Exercise can increase endurance and strengthen the muscles around the joint, making the joint more stable.
Lose weight: Being overweight or obese increases the stress on weight-bearing joints, such as the knees and hips. Even a small amount of weight loss can relieve some pressure and reduce pain.
Use heat and cold to manage pain: Both heat and cold can relieve pain in joints. Heat also relieves stiffness, and cold can relieve muscle spasms and pain.
Make sure you also check our other amazing Article on: Rheumatoid Arthritis