Asthma is a chronic inflammatory disorder of the airways associated with a variable (usually reversible) airflow obstruction and enhanced bronchial hyperresponsiveness to a variety of stimuli.
Table of Contents
Causes
Asthma is characterized by the lungs’ extreme reactivity to numerous stimuli. There is mounting evidence that genetics plays a significant part in the disease’s etiology.
Environmental and genetic variables appear to interact to raise the risk of asthma. Viruses, allergies, and irritating gases and particles in the air are all examples of environmental triggers. Each person has a unique reaction to the elements that can cause asthma.
Physiological factors that may trigger or increase asthma symptoms include:
- Viral upper respiratory infections.
- Heavy exercise.
- Untreated conditions such as rhinitis, sinusitis, and gastroesophageal reflux (GERD).
- Drugs: NSAIDs such as aspirin.
- Ibuprofen, acetaminophen, naproxen sodium, and Ketoprofen; statin drugs (cholesterol-reducing medications) and other anti-inflammatory drugs.
- Stress and strong emotions.
- Menstrual cycle/hormone changes.
Common indoor environmental irritants and allergens that can trigger asthma symptoms or an asthma attack include:
- Pet fur or feathers, pet urine, saliva, and dander.
- House-dust mites.
- Cockroach waste and decomposed bodies of dead animals.
- Mold and mildew spores. (leaking plumbing, leaking roof, etc.)
- Tobacco smoke and wood smoke.
- Perfumes, hairsprays, scented lotions, and cologne.
- Air fresheners, incense sticks, and scented candles.
- Cleaning solutions, pesticides, and paint fumes.
The following are examples of common outdoor environmental irritants and allergens that can cause asthma symptoms or an asthma attack:
- Pollen from trees, grasses, and weeds.
- Mold and mildew spores. (wet rotting leaves on the ground)
- Changes in humidity (high humidity).
- Exposure to cold air or hot humid air.
- Industrial emissions, vehicle or truck exhaust, and other air pollutants such as coal dust.
- Ozone: [O3] is a highly reactive form of oxygen that results from sunlight mixing with hydrocarbons (also called volatile organic compounds) and nitrogen oxides released in fuel combustion)
The immune system of the body reacts to proteins found in food, causing food allergies. These proteins are treated by the body as if they were a sickness. Different people react differently to different foods, though some have a higher risk of becoming a trigger.
Food allergies impact 2% to 10% of the population, with children accounting for the majority of the cases. Reactions might happen in a matter of minutes or over several hours. Severe episodes that go undiagnosed and untreated can be fatal.
Based on causes, asthma is divided into two types:
- Intrinsic asthma: Usually develop beyond age 40 and have many causes other than exposure to allergens.
- Extrinsic asthma: Most commonly develop in childhood and is caused by exposure to definite allergens.
Classification of Asthma
Asthma is currently classified based on clinical severity. Asthma patients and clinicians can better manage therapy options and clinical outcomes as a result of this.
Mild Intermittent Asthma:
It affects persons who have daytime symptoms that happen no more than twice a week and nighttime symptoms that happen no more than twice a month. Between exacerbations, these persons are normally asymptomatic, with a normal Peak Expiratory Flow Rate.
Exacerbations can be mild or severe, although they normally last only a few hours to days. They don’t take daily prescriptions for long-term control; instead, they use only short-term medications for immediate comfort.
Mild Persistent Asthma:
It’s marked by daytime symptoms that happen more than twice a week but less than once a day, as well as nighttime symptoms that happen more than twice a month. These people are asymptomatic, although their pulmonary function tests are abnormal. Exacerbations start to put a cap on how much they can do. For long-term control, they normally take one drug every day. When you use drugs for short-term relief on a daily basis, it means you need more long-term treatment.
Moderate Persistent Asthma:
It affects persons who experience daytime symptoms on a daily basis and nighttime symptoms more than once a week. Exacerbations are defined as periods of reduced activity that occur at least twice a week and can last several days. These people take one or two long-acting antidepressants. Daily use of medicines for rapid relief signals the need for extra long-term treatment.
Severe Persistent Asthma:
It is marked by persistent daytime symptoms as well as frequent nighttime symptoms. They have little physical activity, and exacerbations are common. For long-term control, these folks frequently require two drugs per day. Daily use of medicines for rapid relief signals the need for extra long-term treatment.
Pathophysiology
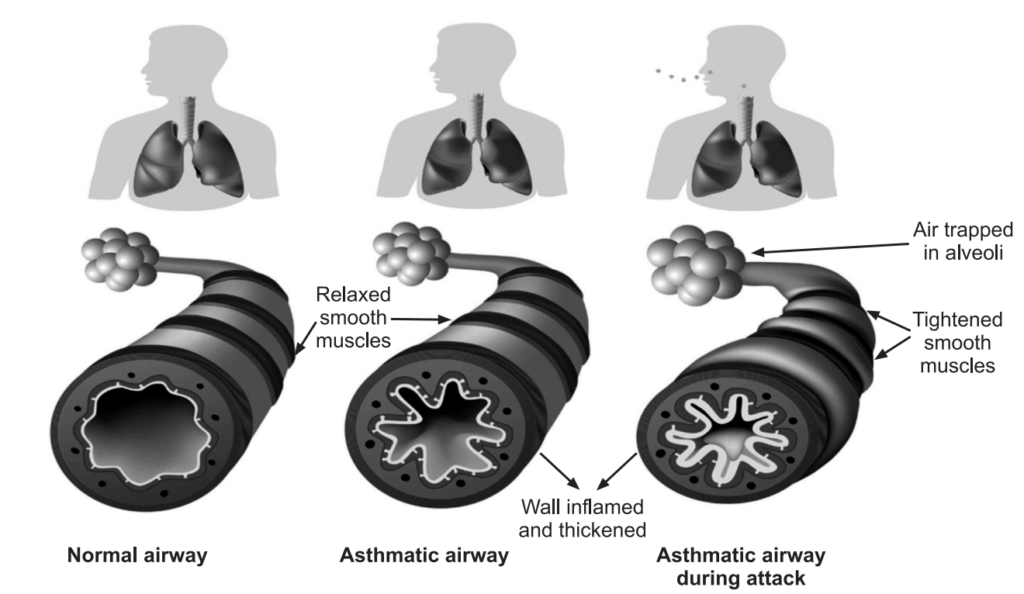
Pollens, dust, mites, certain foods, and certain medicines are some of the frequent allergens that trigger asthma attacks. When allergens are exposed, they cause the creation of IgE, which then binds to mast cells. When exposed to the same allergen again, the allergens quickly attach to IgE, causing mast cell degranulation and the release of inflammatory mediators such as histamine, leukotrienes, and prostaglandins.
WBCs, migrate into the area to absorb the allergens in response to the above alterations. The phagocytic process results in the release of basic proteins, which function as tissue lytic agents and increase inflammation.
With exposure to a trigger, a cascade of cellular responses cause:
- Increased production of thick tenacious mucus with impaired mucociliary function.
- Mucosal swelling due to increased vascular permeability and vascular congestion.
- Bronchial smooth muscle contraction
- These changes cause bronchial hyperresponsiveness and obstruction. Airway obstruction increases resistance to airflow and decreases flow rates, including expiratory flow. Impaired expiration causes hyperinflation distal to the obstruction and increases the work of breathing. These changes are not uniform throughout the lungs but regional. Continued air trapping causes increased intrapleural and alveolar gas pressures resulting in decreased perfusion of the alveoli, the result is hypoxia.
- Late Asthma Response occurs in cases of significant allergen exposure. The symptoms can recur 4 to 12 hours after the initial attack due to persistent cellular activation. It can be more severe than the initial attack.
- Untreated inflammation can cause long-term airway damage that is irreversible (airway remodeling).
Symptoms
Asthma affects the airways, causing them to tighten, become inflamed, or fill with mucus. Asthma symptoms can range from mild to severe. Most people will only experience occasional symptoms, although a few people will have problems most of the time and including:
- Coughing, especially at night, during exercise, or when laughing.
- Shortness of breath.
- Chest tightness.
- Wheezing (a whistling or squeaky sound in the chest when breathing, especially while exhaling).
- Any asthma symptom is serious and can become deadly if left untreated.
- Symptoms may be triggered by exposure to an allergen (such as ragweed, pollen, and pet hair or dust mites), irritants in the air (such as smoke, chemical fumes, or strong odors), or extreme weather conditions.
Diagnosis
Exacerbations of asthma symptoms are a measure of a person’s asthma control. Early detection and correct diagnosis are required to rule out other diseases and reasons for breathing trouble in order to prevent the long-term effects of airway remodeling. Chronic obstructive lung illness, congestive heart failure, pulmonary embolisms, and mechanical obstruction are only a few examples (from tumors).
An asthma diagnosis is based on several factors, including a detailed medical history, a physical exam, symptoms, overall health, and test results.
Medical History and Physical Examination:
The first step in diagnosing asthma is to look for signs of asthma or allergies. These signs include wheezing (high-pitched whistling sounds when breathing out) and a runny nose or swollen nasal passages, and allergic skin conditions (such as eczema).
Lung Function Tests:
Lung function tests are asthma tests that assess lung function. The two most common lung function tests used to diagnose asthma are spirometry and methacholine challenge tests.
Asthma and COPD (Chronic Obstructive Pulmonary Disease) causes problems by narrowing the bronchial tubes (or airways), resulting in shortness of breath. Narrowed airways are difficult to breathe through. The greater the narrowing, the more difficult breathing becomes.
Spirometry:
It is a simple breathing test that is of great value for measuring exactly how much bronchial tubes have narrowed. The spirometer measures the amount (volume) and speed (flow) of air that can be inhaled and exhaled, giving an indication of how well the lungs are performing. It is often used to determine the amount of airway obstruction. This enables one to make decisions about lung conditions and to plan the best treatment for asthma.
Methacholine Challenge Test:
Adults are more likely than children to get this lung function test for asthma. If symptoms and screening spirometry do not clearly or conclusively establish an asthma diagnosis, it may be used. Methacholine is a substance that, when inhaled, causes asthmatic airways to spasm (contract involuntarily) and narrow. A methacholine challenge test is a form of bronchoprovocation test that assesses lung function following exposure to substances that typically cause wheezing and other asthma symptoms.
The purpose of the Methacholine Challenge Test is:
- To identify bronchial hyperresponsiveness in people who have normal results on standard pulmonary function tests.
- To diagnose mild asthma in some atypical cases, such as persistent cough
- To diagnose occupational (workplace) asthma caused by certain dust or chemicals.
- To help determine the risk of developing asthma, evaluate asthma severity, and assess response to asthma treatment.
- To evaluate the effectiveness of asthma medications and determine the risk of developing asthma in the future.
Exhaled Nitric Oxide Test:
It is a quick and easy way to measure inflammation (swelling) in the bronchial tubes of the lungs. During inflammation, higher than normal levels of nitric oxide (NO) are released from epithelial cells of the bronchial wall. The concentration of NO in exhaled breath, or fractional exhaled nitric oxide (FeNO), can help to identify airway inflammation, and thereby support a diagnosis of asthma when other objective evidence is lacking.
Allergy Tests:
Allergy skin tests are vital in finding out whether asthma is due to inhalant allergens. Drops of a number of allergen extracts are placed on the skin (usually the forearm) and the skin is pricked lightly through the drops. A positive reaction will cause some itching and a bump at the site within 10 minutes.
A blood test for allergic antibodies to various allergens is an alternative but in some cases can be less likely to detect an allergy than skin tests.
Prevention and Treatment
Prevention of exposure to known triggers is warranted. Hyposensitization may be beneficial if asthma has an allergic mechanism, in such cases:
- Identify and avoid asthma triggers.
- Identify and treat attacks early and monitor breathing.
- Other measures include a dust-free house.
- Intake of selective type of food.
- Avoid exposure to extreme cold conditions.
- Get vaccinated for influenza and pneumonia.
Pharmacological Treatment:
Drug therapy depends on the frequency and severity of attacks. The bronchodilators are often considered rescue inhalers, while the other medications are considered more prophylactic or therapeutic medications.
Bronchodilators (Sympathomimetics): The mechanism of action for sympathomimetic bronchodilators is to bind the receptors in airway smooth muscle thus causing bronchodilation and increased ciliary beat frequency. e.g. Albuterol, Salbutamol and Terbutaline.
Anticholinergic agents: The effect of anticholinergic bronchodilators is bronchodilation through inhibition of bronchoconstriction secondary to blockade of the effects of acetylcholine. The mechanism of action for anticholinergic bronchodilators is non-selective antagonism of muscarinic receptors leading to downregulation of cGMP which results in bronchodilation. Additional acetylcholine is released in response, thus overcoming the effect on smooth muscle. e.g. Ipratropium, Aclidinium.
Corticosteroids: The effect of inhaled corticosteroids is reduced airway inflammation. Overall airway bronchial hyper-responsiveness decreases. Improved asthma control and increased sensitivity of β-receptors in smooth muscle. The mechanism of action for inhaled corticosteroids is to suppress granuloma formation, reduce arachidonic acid metabolism, up-regulate β-adrenergic receptors on leukocytes, and decrease the synthesis of prostaglandins and leukotrienes. e.g. Beclomethasone, Flunisolide, Triamcinolone.
Biologic Response Modifiers (Monoclonal Antibodies): The effect of Biologic Response Modifiers is decreased frequency of allergen-induced asthma exacerbations. The mechanism of action for Biologic Response Modifiers is, when the monoclonal antibody binds to IgE, interferes with mast cell binding. This prevents mast cell degranulation and the release of inflammatory mediators. Cytokine release seen in the late phase of an allergic reaction is also prevented by blocking the receptors on dendritic cells, epithelial cells, eosinophils, monocytes, and platelets. E.g. Omalizumab.
Leukotriene Receptor Antagonists: The effect of leukotriene receptor antagonists in the prevention of allergen-induced bronchoconstriction. The mechanism of action for leukotriene receptor antagonists is antagonism of cysteinyl-leukotriene receptors, thus preventing histamine release. e.g. Montelukast and Zafirlukast.
Mast Cell Stabilizers: The effect of mast cell stabilizers is the prevention of bronchoconstriction and inflammation. The mechanism of action of mast cell stabilizers is to antagonize mast cell degranulation to prevent the release of histamine and other mediators of allergic reaction. Agents do not interfere with IgE. The anti-inflammatory mechanism is unknown. e.g. Cromolyn and Nedocromil.
Methylxanthine Derivatives: The mechanism of action for methylxanthine derivatives is bronchodilation. The mechanisms of action include prostaglandin antagonism, stimulation of endogenous catecholamines, inhibition of calcium influx into smooth muscle (preventing muscle contraction), antagonism of adenosine receptors, and inhibition of release of mediators from leukocytes and mast cells. E.g. Theophylline.
Make sure you also check our other amazing Article on: Angina Pectoris
