Angina Pectoris is a symptom of myocardial ischemia and occurs due to an imbalance between oxygen demand and oxygen supply of the myocardium.
- Characteristic abrupt, severe, pressing-like substernal chest pain radiating towards neck, jaw, back, and arms. Patients may also experience dyspnea or atypical symptoms such as indigestion, nausea, vomiting, or diaphoresis.
- Usually precipitated by exercise, excitement, or a heavy meal.
- Transient episodes (15 seconds to 15 minutes) of myocardial ischemia (stable angina) do not result in cellular death; as occurs in myocardial infarction (MI).
Table of Contents
TYPES OF ANGINA
Typical Angina (Classical Angina)
- Pain is commonly induced by exercise, excitement, or a heavy meal.
- Secondary to advanced atherosclerosis of coronary vessels.
- Associated with ST-segment depression on ECG.
- Usually lasts 1-15 minutes
Variant Angina (Prinzmetal Angina)
- Pain is induced while at rest.
- Symptoms are caused by decreased blood flow to the heart muscle from the spasm of the coronary artery.
- Although individuals with this form of angina may have significant coronary atherosclerosis, the angina attacks are unrelated to physical activity, heart rate, or blood pressure.
- Associated with ST-segment elevation on ECG.
- Generally responds promptly to coronary vasodilators, such as nitroglycerin and calcium-channel blockers.
- But β-blockers are contraindicated.
Unstable angina (Acute Coronary Syndrome)
- May involve coronary spasm and may also have the component of atherosclerosis.
- The duration of manifestation is longer than the first two and has the manifestation of myocardial infarction (MI).
- Lies between stable angina and MI.
- The pathology is similar to that involved in MI: a platelet-fibrin thrombus associated with a ruptured atherosclerotic plaque but without complete occlusion of the blood vessel.
CLASSIFICATION OF ANTI-ANGINAL DRUGS
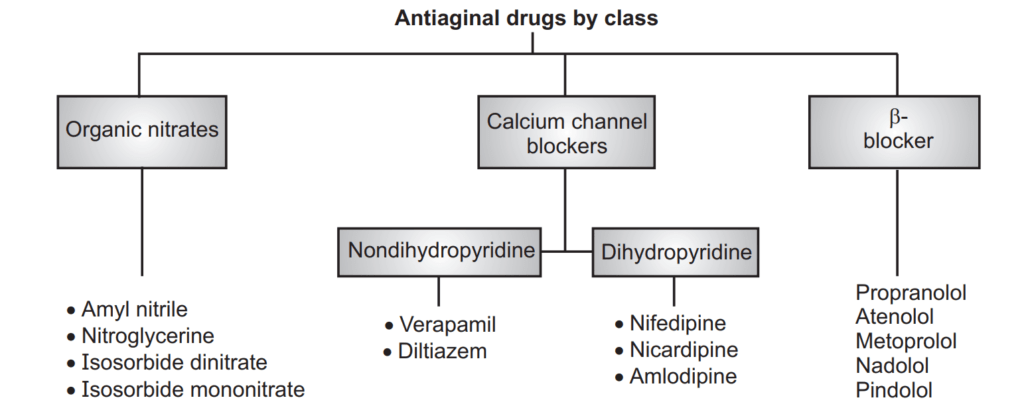
Nitrates/Organic Nitrates
Nitroglycerine, Isosorbide dinitrate, Isosorbide mononitrate.
- Preload reduction: Peripheral pooling of blood → decreased venous return (preload reduction).
- After load reduction: Nitrates also produce some arteriolar dilation → slightly decreasing total peripheral resistance or after load on the heart.
- Redistribution of coronary flow: In the arterial tree, nitrates preferentially relax bigger conducting coronary arteries than arterioles or resistance vessels.
MOA:
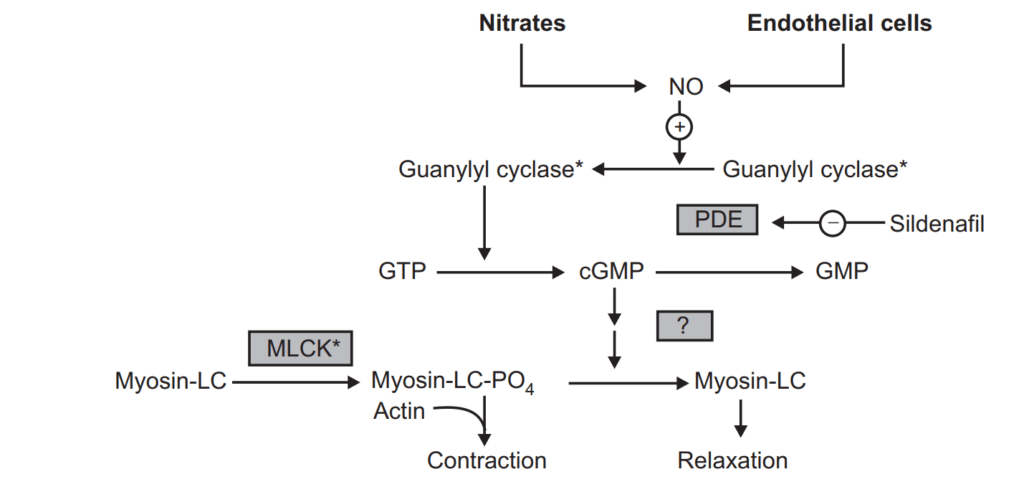
The organic nitrate agents are prodrugs that are sources of NO. NO activates the soluble isoforms of guanylyl cyclase, thereby increasing intracellular levels of cGMP. In turn, cGMP promotes the dephosphorylation of the myosin light chain and the reduction of cytosolic Ca++ and leads to the relaxation of smooth muscle cells in a broad range of tissues.
Adverse effects:
- Headache is the most common adverse effect of nitrates. High doses of nitrates can also cause postural hypotension, facial flushing, and tachycardia.
- Phosphodiesterase type 5 inhibitors such as sildenafil potentiates the action of the nitrates. To preclude the dangerous hypotension that may occur, this combination is contraindicated.
Tolerance:
Tolerance to the action of nitrates develops rapidly as the blood vessels become desensitized to vasodilation. Tolerance can be overcome by providing a daily “nitrate-free interval” to restore sensitivity to the drug.
Dependence:
Sudden withdrawal after prolonged exposure has resulted in spasms of coronary and peripheral blood vessels. Withdrawal of nitrates should be gradual.
β-Blockers
Atenolol, Bisoprolol, Metoprolol, Propranolol
- Atenolol, metoprolol, propranolol, and bisoprolol are used only for prophylactic therapy of angina; they are of no value in an acute attack.
- Effective in preventing exercise-induced angina.
- But are ineffective against the vasospastic form.
- Cardioselective β-blockers, such as metoprolol or atenolol, are preferred. Thus, Propranolol is not preferred.
- Agents with intrinsic sympathomimetic activity (for example, pindolol) are less effective and should be avoided in angina.
The dose should be gradually tapered off over 5 to 10 days to avoid rebound angina or hypertension.
MOA: Suppress the activation of the heart by blocking B1 receptors
- Decrease the heart rate, resulting in:
- decreased myocardial oxygen demand.
- Increased oxygen delivery to the heart.
- Decrease myocardial contractility, helping to conserve energy/ decrease demand.
- Reduce the work of the heart by decreasing COP and causing a slight decrease in BP
- ↓ HR, • ↓ contractility, • ↓ systolic wall tension, • ↑ perfusion time
Reasons for Using Nitrates and β-Blockers in Combination in Angina
- β-Blockers prevent reflex tachycardia and contractility produced by nitrate-induced hypotension.
- Nitrates prevent any coronary vasospasm produced by β- Blockers.
- Nitrates prevent increases in left ventricular filling pressure or preload resulting from the negative inotropic effects produced by β-Blockers.
Calcium Channel Blockers (CCBs)
Amlodipine, Diltiazem, Felodipine, Nicardipine, Nifedipine, Verapamil
MOA:
- Calcium is essential for muscular contraction.
- The CCBs protect the tissue by inhibiting the entrance of Ca+2 into the cardiac and smooth muscle cells of the coronary and systemic arterial beds.
- All CCBs are therefore arteriodilators that cause a decrease in vascular resistance. Cause peripheral arterial vasodilation.
- Reduce myocardial contractility (-ve inotropic action).
- Result: decreased myocardial oxygen demand.
Pharmacological actions:
Smooth muscle: The CCBs cause relaxation by decreasing the intracellular availability of Ca++. Dihydropyridines (DHPs) have the most marked smooth muscle relaxant and vasodilator action; verapamil is somewhat weaker followed by diltiazem.
Heart: Calcium influx is increased in ischemia because of the membrane depolarization that hypoxia produces. The calcium channel blocker protects the tissue by inhibiting the entrance of calcium into cardiac and smooth muscle cells of the coronary and systemic arterial beds and decreases smooth muscle tone and vascular resistance, afterload.
Calcium Channel Blockers: Phenyl alkylamine: Verapamil:
- It dilates arterioles and decreases total peripheral resistance.
- It slows atrioventricular (AV) conduction directly and decreases heart rate, contractility, blood pressure, and oxygen demand.
- It also has some α adrenergic-blocking activity.
- Verapamil has greater negative inotropic effects than amlodipine, but it is a weaker vasodilator.
- Verapamil should not given with β blocker, digoxin, cardiac depressants like quinidine and disopyramide
Benzothiazepines: Diltiazem:
- Diltiazem also slows AV conduction, decreases the rate of firing of the sinus node pacemaker, and is also a coronary artery vasodilator.
- Diltiazem can relieve coronary artery spasms and is particularly useful in patients with variant angina.
- It is a somewhat less potent vasodilator than nifedipine and verapamil and has modest direct negative inotropic action, but direct depression of SA node A-V conduction is equivalent to verapamil.
Dihydropyridine (DHP) Calcium channel blockers:
Nifedipine:
- Nifedipine is the prototype DHP with a rapid onset and short duration of action. It causes arteriolar dilation and decreases total peripheral resistance.
- Nifedipine is usually administered as an extended-release oral formulation.
- It causes direct depressant action on the heart in higher doses.
ADR: Frequent side effects are palpitation, flushing, ankle edema, hypotension, headache, drowsiness, and nausea. Nifedipine has paradoxically increased the frequency of angina in some patients.
Other dihydropyridine (DHP) calcium channel blockers:
- Amlodipine, an oral dihydropyridine, functions mainly as an arteriolar vasodilator.
- Nitrendipine is a calcium channel blocker with additional action of vasodilation action. Vasodilation action is due to the release of NO from the endothelium and inhibits cAmp phosphodiesterase.
- Lacidipine is a highly vasoselective newer DHP.
- Nimodipine is a short-acting DHP that penetrates the blood-brain barrier very efficiently due to high lipid solubility.
- DHP with long duration of action: Lercanidipine, Benidipine.
Uses:
- Calcium channel blockers can be safely given to patients with obstructive lung disease and peripheral vascular disease in whom β blockers are contraindicated.
- CCB is used for the treatment of:
- Angina pectoris
- Hypertension
- Cardiac arrhythmias
- Hypertrophic cardiomyopathy
ADR: Lightheadedness. Low blood pressure. Slower heart rate.
Potassium Channel Openers:
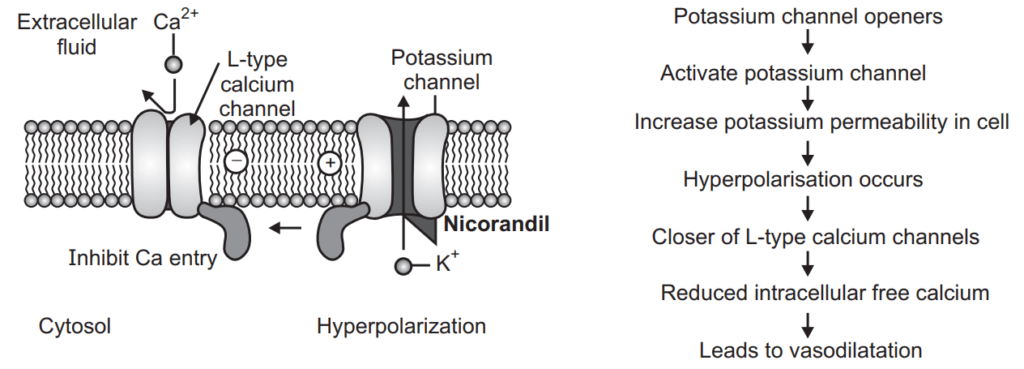
Nicorandil:
- The Antianginal action of nicorandil is mediated through ATP-sensitive K+ channels (KATP) thereby hyperpolarizing vascular smooth muscles.
- Nicorandil is well absorbed orally, nearly completely metabolized in the liver, and excreted in urine. Administered I.V. during angioplasty for acute MI, it is believed to improve outcome.
ADR: Flushing, palpitation, weakness, headache, dizziness, nausea and vomiting.
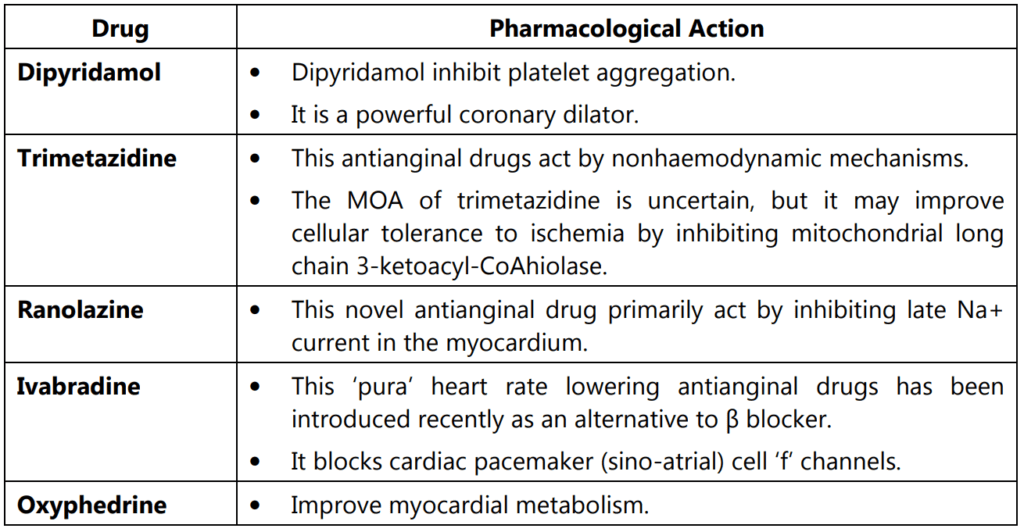
OTHER ANTIANGINAL DRUGS
Make sure you also check our other amazing Article on: Cilnidipine
