Table of Contents
Lungs
There are two lungs. They are cone-shaped organs that lie in the thoracic cavity. The lungs are separated by the heart and the great blood vessels. The space between the two lungs is called the mediastinum. Each lung has an apex and a base. The lungs are convex on the outer surface and concave on the inner surface. The right lung is divided into three lobes, i.e. superior lobe, the middle lobe, and the inferior lobe. The left lung is divided into two lobes, i.e. superior lobe and the inferior lobe.
The convex surface of the lung which is called the costal surface is smooth and follows the shape of the chest wall. The concave surface is called the medial surface.
The lung is covered by a serous membrane known as the pleura, which is composed of epithelial cells. The pleura is divided into two layers:
- Parietal pleura
- Visceral pleura
The parietal pleura lines the ribs, sternum, costal cartilage, and the intercostal muscle fibers and also covers the superior surface of the diaphragm. The visceral pleura is completely attached to the lungs covering the lung surface. It also enters into fissures, assists in dividing the lungs into respective lobes. At the base of the lung, it is reflected backward to form parietal pleura. The flattened epithelial cells secrete a serous fluid which occupies the space between the two layers, i.e. the pleural cavity. This fluid reduces friction between the two membranes and allows them to slide easily over one on another during respiration. The internal structure of the lung shows bronchi, bronchioles, alveolar ducts, alveoli, pulmonary artery, and bronchial artery, branches of the vagus nerve, pulmonary veins, bronchial veins, and lymphatic vessels. These structures occupy the lobules of the lungs. The lobules are separated by interlobular tissue i.e. areolar and elastic tissues. The pulmonary artery brings the venous blood from the right ventricle to the lungs and after entering it divides into many branches in lung tissues. In the end, they form a network of capillaries around the walls of the alveoli. Thus, the exchange of gases takes place through the capillary membrane and alveolar wall. The pulmonary capillaries join up to form pulmonary veins which convey oxygenated blood to the left atrium of the heart.
Mechanism of breathing
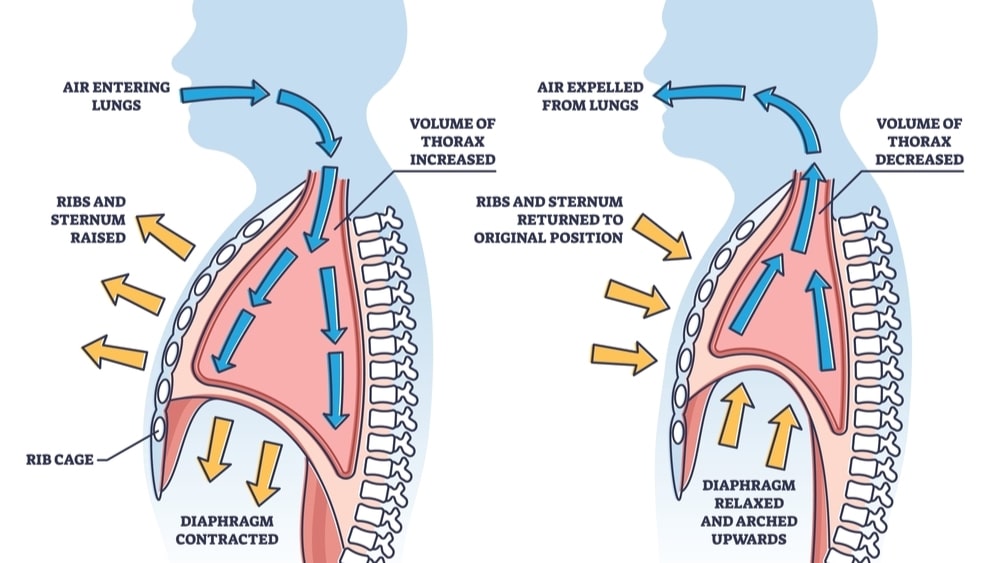
Explain the mechanism of Breathing, When the lungs expand air from the atmosphere it enters the lungs and upon contraction of the lungs, the air is expelled out. The pressure gradient assists in breathing. When the pressure inside the lungs is less than the atmospheric pressure air enters the lungs while when the pressure inside the lungs is greater than the atmospheric pressure, the air moves out of the lungs.
This mechanism occurs in three phases.
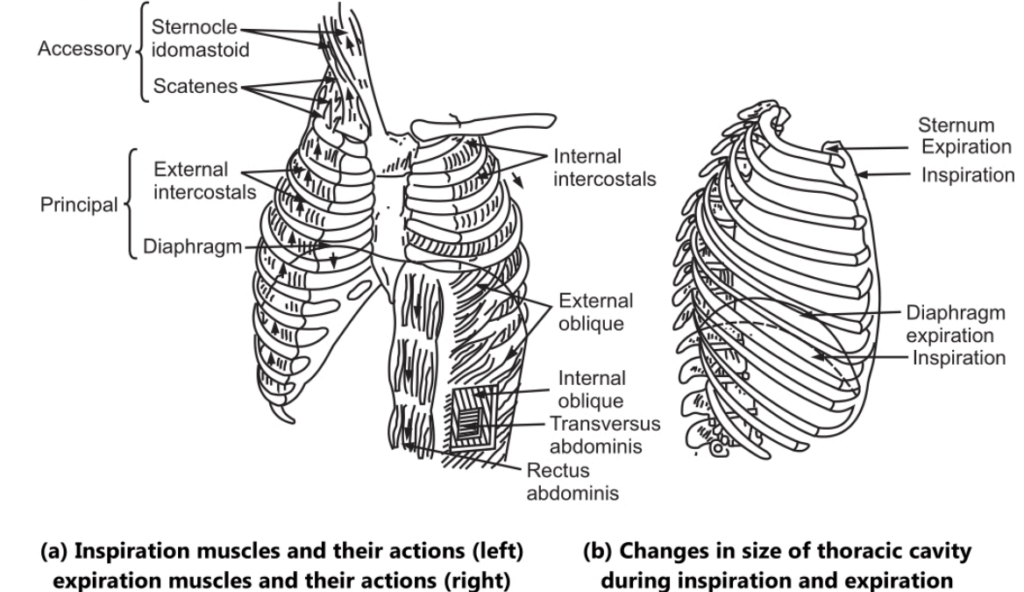
Aspiration phase: The respiration cycle occurs about 16 times/minute. As a result of muscular activity, the chest expands during inspiration. This activity may be partly voluntary and partly involuntary Two types of muscles take part in respiration.
The intercostal muscle: The space between each of the twelve pairs of ribs is called the intercostal space. This space is occupied by muscle fibers. These muscle fibers are arranged in two layers.
The internal intercostal muscle fiber: It is extended in a downward and backward direction between two ribs. In this way, these two muscle fibers form a network or cross pattern occupying intercostal spaces. There is no movement of the first rib; it is immovably attached to the thoracic vertebra and the manubrium. When intercostal muscles contract, they pull all the ribs towards the first rib. Due to the curvy nature of the ribs, when they move upward, they also move outwards. This helps to enlarge the thoracic cavity. These muscle fibers are stimulated by intercostal nerves.
The diaphragm: Due to the relaxation of the diaphragm the thoracic cavity is separated from the abdominal cavity. But when the diaphragm contracts, it is pulled downwards to its original position helps in enlarging the thoracic cavity in length. During contraction, the diaphragm exerts pressure on the abdominal organs and the abdominal wall which moves under this pressure.
The diaphragm is stimulated by phrenic nerves. Due to the simultaneous contraction of intercostal muscles and the diaphragm, the thoracic cavity enlarges in all directions. The parietal pleura are closely attached to the ribs; intercostal muscles and the diaphragm. When all these muscles contract for enlargement of the thoracic cavity, the parietal pleura moves with the thoracic wall. As there is negative pressure between the parietal and visceral pleura, the visceral pleura also moves along with the parietal pleura. As the visceral pleura is closely attached to the lungs, the lungs also stretch. The elastic nature of the tissues of the lungs facilitates this. The lobules of lungs containing bronchi, bronchioles also stretch. The capacity of the lungs increases. Air then enters the lungs. Thus, inspiration occurs. This is an active process. This process takes place due to the existence of a pressure gradient.
Expiration: Breathing out of the air is called expiration. Expiration also results due to a pressure gradient. The pressure inside the lungs is greater than the atmospheric pressure. This is a passive process because no contraction of muscles occurs. There is relaxation of intercostal muscles, causing the ribs to fall back to their original position. Relaxation of the diaphragm occurs and the dome-shaped muscles move upward. Due to the presence of elastic tissue in the lungs, the lungs recoil to expel air. Thus expiration occurs.
After these two processes, there is a short pause.
Exchange of gases at the lung and tissue level: No ATP is used for the exchange of O2 and CO2. This is a passive process.
Dalton’s law: Every gas is a mixture of gases and exerts its own pressure. The pressure exerted by a specific gas in a mixture is called its partial pressure and is denoted by the letter ‘P’. Atmospheric air is a mixture of several gases, like O2, CO2, N2, water vapor (H20), and small quantities of other gases. So the sum of the partial pressures of all gases gives the atmospheric pressure.
Atmospheric Pressure (760 m.g) = pO2 + pCO2 + pN2 + pH2O
We can find out the partial pressure exerted by each gas in a mixture. Multiply the percent of gas with the total pressure of the mixture.
As regards partial pressure of O2 in the atmosphere, the percentage of O2 in atmospheric pressure is 21 percent; multiply it by total atmospheric pressure, i.e. 760 mm Hg.
Atmospheric pressure of pO2 = 0.21 x 760 mm Hg = 159.6 or 160 mm Hg.
Atmospheric pressure of CO2 = 0.0004 x 760 mm Hg = 0.3 mm Hg.
Partial pressures are important in finding out the movement of O2 and CO2 between the atmosphere and lungs, the lungs and blood, and blood and body tissues. Each gas diffuses from the area where its partial pressure is greater to the area where its partial pressure is less. The partial pressures of O2 and CO2 in mm Hg in air, blood, and tissue cells are as follows:
Atmosphere (at sea level) pO2 = 160, PCO2 = 0.3
Alveoli pO2 = 105; pCO2 = 40
Oxygenated blood pO2 = 100, PCO2 = 40
Tissue cells at rest pO2 = 40, pCO2 = 45
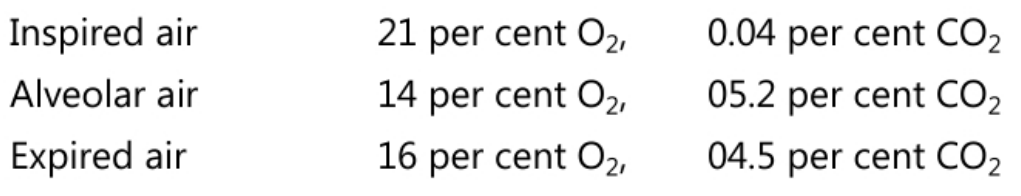
The relative amounts of O2 and CO2 differ in alveolar air, inspired air, and expired air.
The relative amounts of O2 and CO2 differ in alveolar air, inspired air, and expired air.
The O2 in inspired and expired air is more than in alveolar air while CO2 in alveolar air is more than that in inspired and expired air.
External respiration: It is the exchange of O2 and CO2 between the air in the alveoli of the lungs and blood in pulmonary capillaries. In this process, deoxygenated blood is converted to oxygenated blood. The oxygenated blood goes to the heart. The pO2 of alveolar air is 105 mm Hg but at rest pO2 of deoxygenated blood passing through the pulmonary capillary is about 40 mm Hg and during exercise, it is even lower. Due to this difference in pO2 there is a net diffusion of Oz from the alveoli into deoxygenated blood until equilibrium is reached. Here oxygenated blood has pO2 105 mm Hg but the poz of blood in pulmonary veins is about 100 mm Hg. As the O2 diffuses from alveoli into deoxygenated blood, at the same time CO2 diffuses in the opposite direction. The deoxygenated blood has pCO2 45 mm Hg in the resting period and pCO2 of alveolar air is 40 mm Hg. Because of this difference in pressure, CO2 diffuses from deoxygenated blood into alveoli until pCO2 of blood decreases to 40 mm Hg.
External respiration depends upon several factors:
- The partial pressure difference of gases: Because of higher alveolar pO2 than in pulmonary capillaries, O2 diffuses from alveoli into the blood. But at higher altitudes, total atmospheric pressure decreases. As the pO2 of inspired air decreases, alveolar pO2 decreases. Hence less O2 will diffuse into the blood. Common signs of high altitude sickness are shortness of breath, headache, fatigue, insomnia, nausea, and dizziness. This occurs because of the low O2 content of the blood.
- The surface area of gas exchange: As the surface area is large, diffusion may occur in a large area.
- Diffusion distance: The thickness of the alveolar capillary membrane is 0.5 um. Thicker the membrane slower is the rate of diffusion.
- Solubility of Molecular weight: O2 has a low molecular weight than CO2. So 02 diffuses across the membrane 01.2 times faster than CO2. CO2 has 24 times more solubility than O2 in the fluid portion of the alveolar-capillary membrane; hence net outward diffusion of CO2 occurs 20 times more rapidly than net inward O2 diffusion.
- Internal respiration: The exchange of O2 and CO2 between tissue, blood capillaries, and tissue cells is called internal respiration. Oxygenated blood entering the tissue capillaries has a pO2 of 100 mm Hg, whereas tissue cells have an average po2 of 40 mm Hg. Due to this difference of pO2, O2 diffuses from oxygenated blood into interstitial fluid and then into tissue cells until poz in the blood decreases to 40 mm Hg.
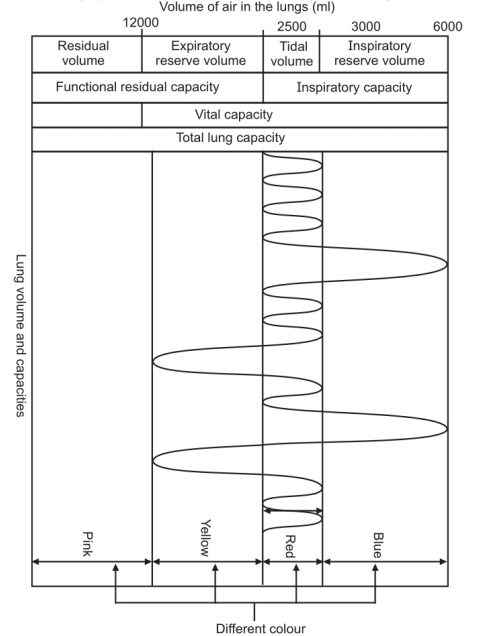
- The Lung Capacity: The rate of respiration and depth of breathing can change considerably depending upon the activity and emotional state of the individual. Hence, the amount of air that passes in and out of the lungs also varies according to the depth of respiration.
- Tidal Volume: When an individual is in a normal, quiet breathing state, approximately 500 ml of air passes into and out of the lungs. This is the volume of one breath and is known as the tidal volume.
Inspiratory Reserve Volume
During forced inspiration, the amount of air which can be taken into the lungs is called as aspiratory reserve volume. This amount is approximately 1500 ml
Expiratory Reserve Volume
The Vital Capacity: It is the sum of the aspiratory reserve volume, tidal volume, and expiratory reserve volume. Thus, it is the largest volume of air which can be expired after the deepest possible inspiration. This volume is approximately 3500 ml.
Residual Volume: Even after the deepest possible expiration, a certain amount of air remains present in the respiratory passage. This is called as the residual volume. The volume of air can be measured by spirometry. This amount is approximately 1500 ml.
Make sure you also check our other amazing Article on: Pulmonary Ventilation