AIDS (Acquired Immunodeficiency Syndrome) is a chronic, potentially life-threatening condition caused by the human immunodeficiency virus (HIV). By damaging the immune system, HIV interferes with the body’s ability to fight against the organisms that cause disease.
Acquired immunodeficiency syndrome (AIDS) is defined in terms of either a CD4+ T cell count below 200 cells per µL (CD4 lymphocyte percentage below 14% are considered to have AIDS) or the occurrence of specific diseases in association with an HIV infection. AIDS is the most advanced stage of infection with HIV.
HIV stands for human immunodeficiency virus:
H – Human: This particular virus can only infect human beings.
I – Immunodeficiency: HIV weakens the immune system by destroying important cells that fight disease and infection.
V – Virus: A virus can only reproduce itself by taking over a cell in the body of its host.
The virus can be isolated from body fluids, blood, semen, vaginal secretion, saliva, breast milk, tears, urine, cerebrospinal fluid, peritoneal fluid. An important cause of infection is unsafe sexual intercourse, sharing unsterilized needles, blood, and blood products.
The presence of HIV in saliva, urine, and tears is not significant to transmit infection. The casual, non-sexual contact does not transmit infection. A mosquito bite is also not responsible for the transmission of HIV.
Table of Contents
HIV Structure
It is around 100 to 120 nm in diameter (around 60 times smaller than a red blood cell) and roughly spherical. It is a 20 sided enveloped virus of the lentivirus subfamily of retroviruses.
HIV is different in structure from other retroviruses. Two viral strands of RNA are found in the core surrounded by protein outer coat. The outer envelope contains a lipid matrix within which specific viral glycoproteins are embedded and these knob-like structures are responsible for binding to the target cell.
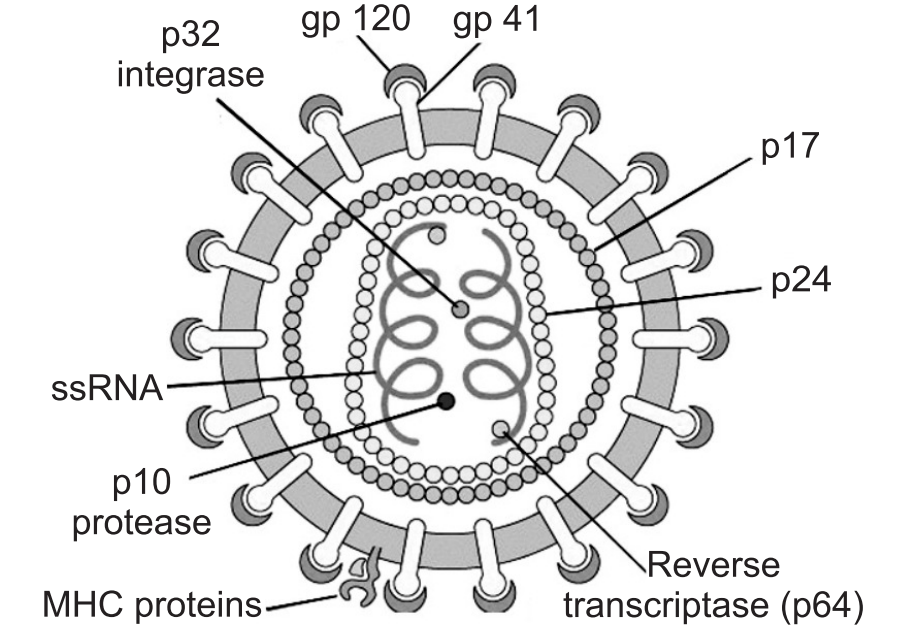
The outer shell of the virus is known as the viral envelope. Embedded in the viral envelope is a complex protein is known as envelope (env) which consists of an outer protruding cap glycoprotein (GP) 120, and a stem gp41. Within the viral envelope is an HIV protein called p17 (matrix), and within this is the viral core or capsid, which is made up of another viral protein p24 (core antigen).
Three main structural genes are Group Specific Antigen (Gag), Envelope (Env), and Polymerase (Pol).
Group-Specific Antigen (Gag): Gag proteins are encoded by the gag gene, and provide structural elements of the virus.
Envelope (Env) gene codes for envelope proteins gp160, gp120 and gp41. These polyproteins will eventually be cleaved by proteases to become HIV envelope glycoproteins gp120 and gp41. gp41 is a transmembrane glycoprotein antigen that spans the inner and outer membranes and attaches to gp120 and both are involved with the fusion and attachment of HIV to CD4 antigen on host cells.
Polymerase (Pol) codes for p66 and p51 subunits of reverse transcriptase and p31 an endonuclease. They are located in the core, close to nucleic acids, and responsible for conversion of viral RNA into DNA, integration of DNA into host cell DNA, and cleavage of protein precursors.
During the first step, HIV attaches to the susceptible host cell. The site of attachment is the CD4 antigen found on a variety of cells, helper T cells, macrophages, monocytes, B cells, microglial brain cells, and intestinal cells. T cells were infected later on.
Pathophysiology
After the virus enters the body there is a period of rapid viral replication, leading to an abundance of virus in the peripheral blood. During primary infection, the level of HIV may reach several million virus particles per milliliter of blood. This response is accompanied by a marked drop in the number of circulating CD4+ T cells. Acute viremia is almost invariably associated with activation of CD8+ T cells, which kill HIV-infected cells, and subsequently with antibody production, or seroconversion. The CD8+ T cell response is thought to be important in controlling virus levels, which peak and then decline, as the CD4+ T cell counts recover. A good CD8+ T cell response has been linked to slower disease progression and a better prognosis, though it does not eliminate the virus.
Ultimately, HIV causes AIDS by depleting CD4+ T cells. This weakens the immune system and allows opportunistic infections. T cells are essential to the immune response and without them, the body cannot fight infections or kill cancerous cells. The mechanism of CD4+ T cell depletion differs in the acute and chronic phases. During the acute phase, HIV-induced cell lysis and killing of infected cells by cytotoxic T cells accounts for CD4+ T cell depletion, although apoptosis may also be a factor.
During the chronic phase, the consequences of generalized immune activation coupled with the gradual loss of the ability of the immune system to generate new T cells appear to account for the slow decline in CD4+ T cell numbers.
Although the symptoms of immune deficiency characteristic of AIDS do not appear for years after a person is infected, the bulk of CD4+ T cell loss occurs during the first weeks of infection, especially in the intestinal mucosa, which harbors the majority of the lymphocytes found in the body. The reason for the preferential loss of mucosal CD4+ T cells is that the majority of mucosal CD4+ T cells express the CCR5 protein which HIV uses as a co-receptor to gain access to the cells, whereas only a small fraction of CD4+ T cells in the bloodstream do so.
A specific genetic change that alters the CCR5 protein when present in both chromosomes very effectively prevents HIV infection.
HIV seeks out and destroys CCR5 expressing CD4+ T cells during acute infection. A vigorous immune response eventually controls the infection and initiates the clinically latent phase. CD4+ T cells in mucosal tissues remain particularly affected. Continuous HIV replication causes a state of generalized immune activation persisting throughout the chronic phase. Immune activation, which is reflected by the increased activation state of immune cells and release of pro-inflammatory cytokines, results from the activity of several HIV gene products and the immune response to ongoing HIV replication. It is also linked to the breakdown of the immune surveillance system of the gastrointestinal mucosal barrier caused by the depletion of mucosal CD4+ T cells during the acute phase of the disease.
Modes of Transmission
Sexual transmission: The most frequent mode of transmission of HIV is through sexual contact with an infected person occurs through unprotected heterosexual contacts. Risk of transmission increases in the presence of many sexually transmitted infections like syphilis, gonorrhea, and genital ulcers.
Exposure to infected blood or blood products: The second most frequent mode of HIV transmission is via blood and blood products through needle-sharing during intravenous drug use, needle stick injury, transfusion of contaminated blood or blood product, or medical injections with unsterilized equipment.
Mother to fetus: HIV can be transmitted from mother to child during pregnancy, during delivery, or through breast milk. This is the third most common way in which HIV is transmitted globally. In the absence of treatment, the risk of transmission before or during birth is around 20%, and in those who also breastfeed 35%. Perinatal transmission is variable and dependent on viral load and mother’s CD 4 count.
Use of contaminated clotting factors by hemophiliacs: People living with hemophilia require regular transfusions of clotting factors in order to maintain a normal blood clotting system. Therefore, those hemophilia patients receiving untested and unscreened clotting factors are at extreme risk for contracting HIV via the blood products.
Transplantation of infected tissues or organs: The risks of transplant-related HIV infection are low. All organ and tissue donors are screened for risk factors and tested for HIV and other infectious agents that potentially could be transmitted through transplantation.
Primary HIV Syndrome:
Most people who have been infected with HIV experience a short, flu-like illness (also known as seroconversion illness) that occurs two to six weeks after infection. It is estimated that up to 80% of people who have been infected with HIV experience this illness. After this, HIV often causes no symptoms for several years. The most common symptoms are fever, sore throat, body rash, headache, diarrhea, tiredness, joint pain, muscle pain, and lymphadenopathy.
Primary HIV syndrome resolves itself and HIV-infected person remains asymptomatic for a prolonged period of time, often years, HIV continues to reproduce, CD4 count gradually declines from its normal value of 500-1200 cells per µL. Once the CD4 count drops below 500 cells per µL, HIV infected person is at risk for opportunistic infections.
Signs and Symptoms of Common Opportunistic Infections include:
- Dry cough or shortness of breath,
- Difficult or painful swallowing,
- Diarrhea lasting for more than a week,
- White spots or unusual blemishes in and around the mouth,
- Pneumonia-like symptoms,
- Shaking chills or fever higher than 100 F (38ºC) for several weeks,
- Vision loss,
- Nausea, abdominal cramps, vomiting,
- Red, brown, pink, or purplish blotches on or under the skin or inside the mouth, nose, or eyelids,
- Seizures or lack of coordination,
- Neurological disorders such as depression, memory loss, and confusion,
- Severe headaches and neck stiffness,
- Coma.
CD4 count drops below 200 cells per µL, a person is considered to have advanced HIV disease:
During late-stage HIV infection, the risk of developing a life-threatening illness is much greater. Examples include:
- Esophagitis (inflammation of the lining of the lower end of the esophagus).
- Infections to the nervous system (acute aseptic meningitis, subacute encephalitis, peripheral neuropathy).
- Pneumonia.
- Some cancers, such as Kaposi’s sarcoma, invasive cervical cancer, lung cancer, rectal carcinomas, hepatocellular carcinomas, head and neck cancers, lymphomas, etc.
- Toxoplasmosis (a disease caused by a parasite that infects the brain. It can also cause disease in the eyes and lungs).
- Tuberculosis. Life-threatening illnesses may be controlled and treated with proper HIV treatment.
If CD4 count drops below 50 cells per µL
- Persistent herpes-zoster infection (shingles),
- Oral candidiasis (thrush),
- Oral hairy leukoplakia,
- Kaposi’s sarcoma (KS),
- Mycobacterium avium,
- Cytomegalovirus infections,
- Lymphoma,
- Dementia.
Most deaths occur with CD4 counts below 50 cells per µL.
Infants with HIV
- Failure to thrive,
- Persistent oral candidiasis,
- Hepatosplenomegaly,
- Lymphadenopathy,
- Recurrent diarrhea,
- Recurrent bacterial infections,
- Abnormal neurologic findings.
Diagnosis
There are several types of tests that screen blood (and sometimes saliva) for HIV infection.
Newer tests can detect the presence of HIV antigen, a protein, up to 20 days earlier than standard tests. It is confirmed by demonstrating certain serological tests.
Performance of medical tests is often described in terms of:
- Sensitivity: The percentage of the results that will be positive when HIV is present.
- Specificity: The percentage of the results that will be negative when HIV is not present. All diagnostic tests have limitations, and sometimes their use may produce erroneous or questionable results.
- False-positive: The test incorrectly indicates that HIV is present in a non-infected person.
- False-negative: The test incorrectly indicates that HIV is absent in an infected person. Tests used for the diagnosis of HIV infection in a particular person require a high degree of both sensitivity and specificity.
Antibody Tests:
The most common HIV tests look for HIV antibodies in the body, rather than looking for HIV itself.
ELISA: The enzyme-linked immunosorbent assay (ELISA) was the first screening test commonly employed for HIV. ELISA tests use blood, oral fluid, or urine to detect HIV antibodies. If the result from either of these tests is positive, will need to take another test, called a Western blot test, to confirm that result. It can take up to two weeks to confirm a positive result.
Western blot test: Like the ELISA procedure, the western blot is an antibody detection test. However, unlike the ELISA method, the viral proteins are separated first and immobilized. In subsequent steps, the binding of serum antibodies to specific HIV proteins is visualized.
Antigen tests: These tests are not as common as antibody tests, but they can be used to diagnose HIV infection earlier from 1-3 weeks after first being infected with HIV. Antigen tests require a blood sample.
PCR test (Polymerase chain reaction test): This test detects the genetic material of HIV itself, and can identify HIV in the blood within 2-3 weeks of infection. Babies born to HIV-positive mothers are tested with a special PCR test because their blood contains their mother’s HIV antibodies for several months. This means they would test HIV-positive on a standard antibody test but a PCR test can determine whether the babies have HIV themselves.
Therapeutic Approach to HIV Infection: There is currently no cure for AIDS or HIV infection. Although antiretroviral treatment can suppress HIV and can delay AIDS-related illness for many years to live a long and healthy life, it cannot clear the virus completely.
A combination of antiretroviral drugs, called antiretroviral therapy (ART), also known as highly active antiretroviral therapy (HAART), is very effective in reducing the amount of HIV in the bloodstream. This is measured by the viral load (how much free virus is found in the blood). Preventing the virus from reproducing (replicating) can improve T-cell counts and help the immune system recover from HIV infection.
In 1987, a drug called Azidothimidine (AZT) became the first approved treatment for HIV disease. Since then, approximately 30 drugs have been approved to treat people living with HIV/AIDS, and more are under development.
e.g. Didinosine, Stavudine, Zalcitabine etc.
The classes of anti-HIV drugs include:
Non-nucleoside reverse transcriptase inhibitors (NNRTIs): NNRTIs disable a protein needed by HIV to make copies of itself. Examples include Efavirenz, Etravirine, and Nevirapine.
Nucleoside reverse transcriptase inhibitors (NRTIs): NRTIs are faulty versions of building blocks that HIV needs to make copies of themselves. Examples include Abacavir and the combination drugs Emtricitabine and Tenofovir and Lamivudine and Zidovudine.
Protease inhibitors (PIs): PIs disable protease, another protein that HIV needs to make copies of itself. Examples include Atazanavir, Darunavir, Fosamprenavir and Ritonavir.
Entry or fusion inhibitors: These drugs block HIV’s entry into CD4 cells. Examples include Enfuvirtide and Maraviroc.
Integrase inhibitors: It is a disabled integrase, a protein that HIV uses to infect CD4+ T cells. The most common integrase inhibitor is Raltegravir.
Prevention
Certain educational and motivational programs can effectively reduce the spread of HIV and AIDS.
Safe sex practice: Such as using latex condoms are effective in preventing HIV transmission. But there is a risk of getting the infection, even with the use of condoms.
Abstain: (Abstain from sex) Not having vaginal, anal, or oral sex is the surest way to avoid HIV. Abstinence or delay of sexual onset can reduce the transmission rate, especially in the young population who have not started the sexual activity.
Drug abuse and needle sharing: Intravenous drug use is an important factor in HIV transmission in developed countries. Sharing needles can expose users to HIV and other viruses. Strategies such as needle exchange programs are used to reduce the infections caused by drug abuse.
Body fluid exposure: Exposure to HIV can be controlled by employing precautions to reduce the risk of exposure to contaminated blood. At all times, health care workers should use barriers (gloves, masks, protective eyewear, shields, and gowns). Frequent and thorough washing of the skin immediately after being contaminated with blood or other bodily fluids can reduce the chance of infection.
Pregnancy: Anti-HIV medicines can harm the unborn child. But an effective treatment plan can prevent HIV transmission from mother to baby. Precautions have to be taken to protect the baby’s health. Breastfeeding may have to give way to bottle feeding if the mother is infected.
Make sure you also check our other amazing Article on: Morphology of Cell Injury
