Chronic Obstructive Airways Disease (COPD) is a lung disease that includes-
- Respiratory failure
- Bronchitis
- Emphysema
Table of Contents
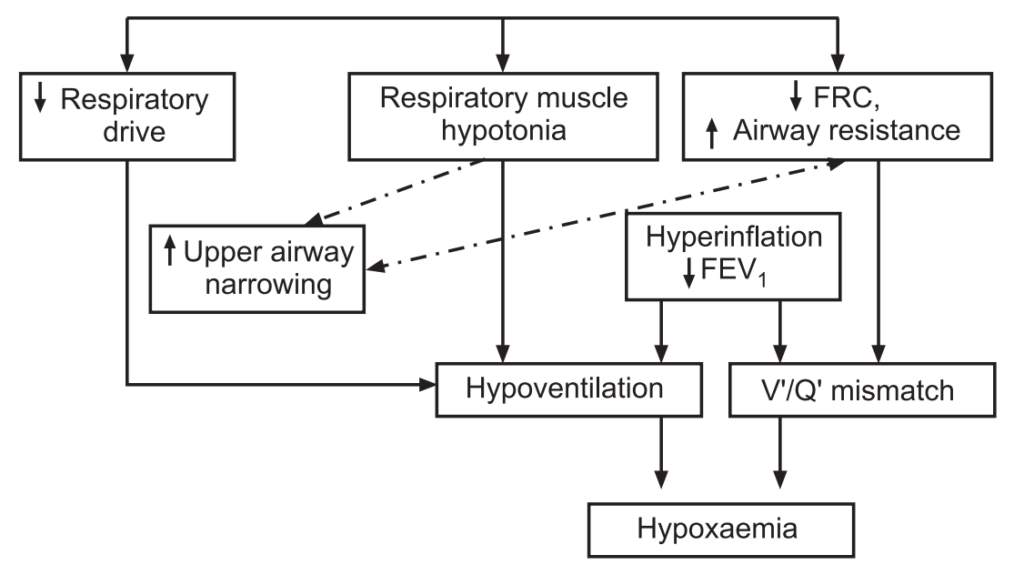
Respiratory Failure
Respiratory failure is the inadequate gas exchange by the respiratory system, with the result that levels of arterial oxygen, carbon dioxide or both cannot be maintained within their normal ranges. A drop in blood oxygenation is known as hypoxemia; a rise in arterial carbon dioxide levels is called hypercapnia. The normal reference values are oxygen PaO2 more than 80 mmHg (11 kPa), and carbon dioxide PaCO2 lesser than 45 mmHg (6.0 kPa). It is classified into type I or type II which relates to the absence or presence of hypercapnia respectively.
Hypoxemic respiratory failure (type I): It is characterized by an arterial oxygen tension (Pa O2) lower than 60 mm Hg with a normal or low arterial carbon dioxide tension (Pa CO2). This is the most common form of respiratory failure, and it can be associated with virtually all acute diseases of the lung, which generally involve fluid filling or collapse of alveolar units. Some examples of type I respiratory failure are cardiogenic or non-cardiogenic pulmonary edema, pneumonia, and pulmonary hemorrhage.
Hypercapnic respiratory failure (type II): It is characterized by a PaCO2 higher than 50 mm Hg. Hypoxemia is common in patients with hypercapnic respiratory failure who are breathing room air. The pH depends on the level of bicarbonate, which, in turn, is dependent on the duration of hypercapnia. Common etiologies include drug overdose, neuromuscular disease, chest wall abnormalities, and severe airway disorders (e.g, asthma and chronic obstructive pulmonary disease).
Respiratory failure may be further classified as either acute or chronic. Acute respiratory failure is characterized by life-threatening derangements in arterial blood gases and acid-base status. The manifestations of chronic respiratory failure are less dramatic and may not be as readily apparent.
Acute hypercapnic respiratory failure develops over minutes to hours; therefore, pH is less than 7.3 (blood). Chronic respiratory failure develops over several days or longer, allowing time for renal compensation and an increase in bicarbonate concentration. Therefore, the pH usually is only slightly decreased.
Causes
Common causes of type I (hypoxemic) respiratory failure include the following:
- COPD
- Pneumonia
- Pulmonary edema
- Pulmonary fibrosis
- Asthma
- Pneumothorax
- Pulmonary embolism
- Pulmonary arterial hypertension
- Pneumoconiosis
- Granulomatous lung diseases
- Cyanotic congenital heart disease
- Bronchiectasis
- Acute respiratory distress syndrome (ARDS)
- Fat embolism syndrome
- Kyphoscoliosis
- Obesity
Common causes of type II (hypercapnic) respiratory failure include the following:
- COPD
- Severe asthma
- Drug overdose, poisoning
- Myasthenia gravis
- Polyneuropathy
- Poliomyelitis
- Primary muscle disorders
- Porphyria
- Cervical cordotomy
- Head and cervical cord injury
- Primary alveolar hypoventilation
- Obesity-hypoventilation syndrome
- Pulmonary edema
- ARDS (adult respiratory distress syndrome)
- Myxedema
- Tetanus
Symptoms
A majority of patients with respiratory failure are shortness of breath. Both low oxygen and high carbon dioxide can impair mental functions. The patients may become confused and disoriented and find it impossible to carry out their normal activities and work.
- Marked CO2 excess can cause headaches and, in time, a semiconscious state, restlessness, anxiety, confusion, seizures, or even coma.
- Low blood oxygen causes bluish coloration in the skin, fingertips, and lips.
- Tachycardia and cardiac arrhythmias may result from hypoxemia and acidosis.
- Polycythaemia is a complication of long-standing hypoxemia.
- Corpulmonale (failure of the right side of the heart): Pulmonary hypertension is frequently present and may induce right ventricular failure, leading to hepatomegaly and peripheral edema.
- Physical examination may show a patient who is breathing rapidly, is restless, and has a rapid pulse.
- Lung disease may cause abnormal sounds; wheezing in asthma, “crackles” in obstructive lung disease.
A patient with ventilatory failure is prone to gasp (catch one’s breath with an open mouth, owing to pain or astonishment) for breath, and may use the neck muscles to help expand the chest.
Complications
- Pulmonary fibrosis.
- Collapsed lung (pneumothorax).
- Blood clots.
- Infections.
- Abnormal lung function.
- Memory, cognitive and emotional problems.
Diagnosis
The symptoms and signs of respiratory failure are not specific. Rather, they depend on what is causing the failure and on the patient’s condition before it developed.
Physical Examination
It includes a history of duration of fever, cough, and sputum. Other signs include open mouth respiration, sweating, the clicking of the tongue, etc. Headache, confusion, and impaired consciousness may result from high levels of carbon dioxide. Cyanosis may result from a low level of oxygen.
Lab Tests:
Arterial blood gas analysis: A test using blood from an artery in the wrist can measure oxygen level. A low level of oxygen or a high level of carbon dioxide in the blood (or both) is a possible sign of respiratory failure. Other types of blood tests can check for signs of infection or anemia.
Complete blood count (CBC): Anaemia can contribute to tissue hypoxia; polycythemia may indicate chronic hypoxaemic respiratory failure.
Renal function tests and Liver function tests: These may provide clues to the etiology or identify complications associated with respiratory failure. Abnormalities in electrolytes such as potassium, magnesium, and phosphate may aggravate respiratory failure and other organ dysfunction.
Serum creatine kinase and troponin I: To help exclude recent myocardial infarction. Elevated creatine kinase may also indicate myositis.
Thyroid function tests: Hypothyroidism may cause chronic hypercapnic respiratory failure.
Spirometry: It is useful in the evaluation of chronic respiratory failure.
Heart tests: The signs and symptoms of respiratory failure are similar to those of certain heart problems.
Echocardiography: If a cardiac cause of acute respiratory failure is suspected.
Pulmonary function tests: These tests are useful in the evaluation of chronic respiratory failure.
ECG: To evaluate a cardiovascular cause; it may also detect dysrhythmias resulting from severe hypoxemia or acidosis.
Right heart catheterization: It should be considered if there is uncertainty about cardiac function, adequacy of volume replacement, and systemic oxygen delivery.
Imaging Tests:
Chest X-ray: A chest X-ray can reveal, which parts of the lungs have fluid in them and whether the heart is enlarged.
Computerized tomography (CT): CT scans can provide detailed information about the structures within the heart and lungs.
Treatment
The goals of treatment for respiratory failure are to increase oxygenation and improve ventilation. Treatment depends on the severity of the respiratory failure and the cause. Acute respiratory failure treatment will address the underlying cause and include ventilation and oxygenation as needed. Exacerbation of chronic respiratory failure by infection may require hospitalization, and treatment may include oxygenation and ventilator support. Bronchodilators may improve airway patency.
Multiple options are available for the treatment of respiratory failure. Examples include:
- Antibiotics to prevent and treat respiratory infections.
- Bi-level positive airway pressure (BiPAP).
- Bronchodilators, like anticholinergics, such as tiotropium, or β-agonists, such as Albuterol.
- Continuous positive airway pressure (CPAP).
- Inhaled steroid medications to decrease inflammation.
- Lung transplant, in rare cases.
- Mechanical ventilation, if oxygen therapy is not sufficient to increase blood oxygen levels.
- Oxygen therapy to increase blood oxygen levels.
- A tracheostomy is a hole made in the front of the neck to help to breathe.
- A patient whose breathing remains very poor will require a ventilator to aid breathing.
- Suctioning the lungs through a small plastic tube passed through the nose, in order to remove secretions from the airways that the patient cannot cough up.
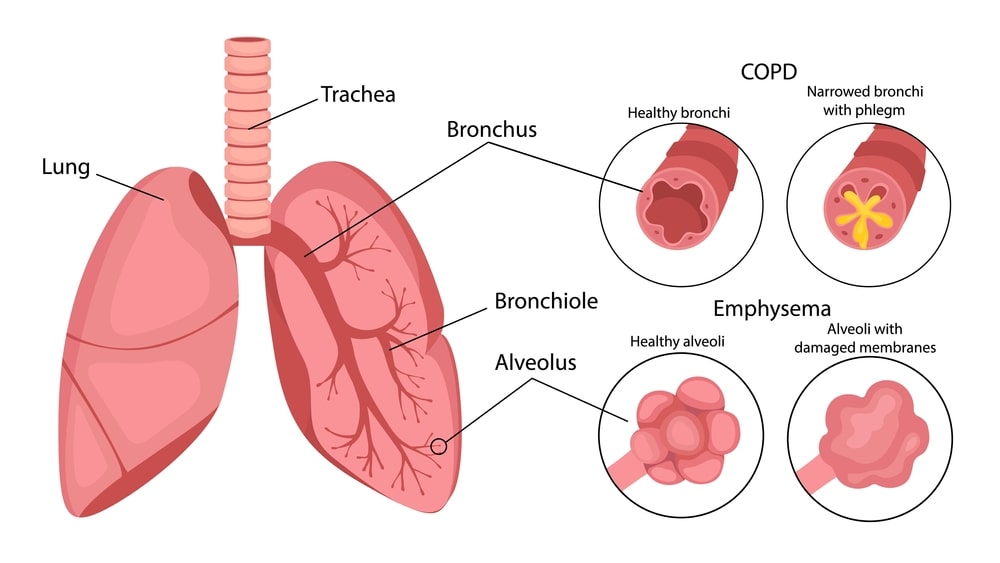
Bronchitis
Bronchitis is an inflammation of the lining of the bronchial tubes, the airways that connect the trachea (windpipe) to the lungs. Bronchitis is more specifically when the lining of the bronchial tubes becomes inflamed or infected. People with bronchitis breathe less air and oxygen into their lungs; they also have heavy mucus or phlegm forming in their airways.
Bronchitis can be acute or chronic. An acute medical condition occurs quickly and can cause severe symptoms, but it lasts only a short time (no longer than a few weeks). Acute bronchitis is most often caused by viruses that can infect the respiratory tract and attack the bronchial tubes. Infection by certain bacteria can also cause acute bronchitis. Most people have acute bronchitis at some point in their lives.
Chronic bronchitis can be mild to severe and is longer lasting from several months to years. With chronic bronchitis, the bronchial tubes continue to be inflamed (red and swollen), irritated, and produce excessive mucus over time. The most common cause of chronic bronchitis is smoking.
Acute Bronchitis
Acute bronchitis is swelling and inflammation of the main air passages to the lungs. This swelling narrows the airways, making it harder to breathe and causing other symptoms, such as a cough.
Causes
Acute bronchitis almost always follows a cold or flu-like infection. The infection is caused by viruses (influenza, parainfluenza, respiratory syncytial virus, rhinovirus, and adenovirus). At first, it affects the nose, sinuses, and throat. Then it spreads to the airways leading to the lungs. Sometimes, bacteria (Mycoplasma, Streptococcus, Bordetella, Moraxella, Haemophilus, and Chlamydia pneumonia) also infect the airways. This is called a secondary infection. In addition, other agents such as tobacco smoke, chemicals, and environmental air pollution may irritate the bronchi and cause acute bronchitis.
Symptoms
The symptoms of acute bronchitis may include:
- Chest discomfort.
- Cough that produces mucus; it may be clear or yellow-green.
- Fatigue.
- Fever, usually low grade.
- Shortness of breath that gets worse with activity.
- Wheezing, in people with asthma.
- Even after acute bronchitis has cleared, a dry and nagging cough may remain for 1 to 4 weeks.
Diagnosis
In acute bronchitis, coughing usually lasts between 10 to 20 days. There are no specific tests for acute bronchitis. Certain tests may be required if there is a recurrent or persistent cough that may suggest asthma or chronic bronchitis. Coughing for a period of greater than four weeks may be due to whooping cough (pertussis).
Sputum tests: Sputum can be tested to see whooping cough (pertussis) or other illnesses that could be helped by antibiotics. Sputum can also be tested for signs of allergies.
- Chest X-ray
- Spirometry
- Pulse oximetry
Treatment
Acute bronchitis usually resolves its own within a couple of weeks, with complete healing of the airways and return to full function. Hence, the aim of treatment is to control symptoms.
Treatment of acute bronchitis involves:
- Getting adequate rest and fluid intake.
- Use of analgesic and antipyretic medications to relieve muscle aches, pains, headaches, and to reduce fever.
- Use of cough suppressants for a dry cough, but not for a productive cough.
- Use of expectorants for productive cough, to help clear the airways of mucus.
- Stopping smoking and avoidance of other airborne irritants.
Bronchitis usually results from a viral infection, so antibiotics are not effective.
Antibiotics: Sometimes bacteria may also infect the airways along with the virus.
Cough medicine: It is best not to suppress a cough that brings up mucus because coughing helps to remove irritants from the lungs and air passages.
Other medications: Use bronchodilators like ipratropium bromide, theophylline to open obstructed airways in people who have associated wheezing with their coughing or underlying asthma or COPD.
Chronic Bronchitis
Chronic bronchitis is a long-term, often irreversible respiratory illness. It is a chronic inflammatory condition in the lungs that causes the respiratory passages to be swollen and irritation increases mucus production and damages the lungs.
Causes
Bronchitis is considered “chronic” if symptoms continue for three months or longer. Bronchitis caused by allergies can also be classified as chronic bronchitis.
There are many causes of chronic bronchitis, but the main cause is cigarette smoke.
Many other inhaled irritants (for example, smog, industrial pollutants, toxic gases in the environment or workplace, and solvents) can also result in chronic bronchitis.
Viral and bacterial infections that result in acute bronchitis may lead to chronic bronchitis if people have repeated attacks with infectious agents. Also, underlying disease processes (for example, asthma, cystic fibrosis, immunodeficiency, congestive heart failure, familial genetic predisposition to bronchitis, and congenital or acquired dilation of the bronchioles) may cause chronic bronchitis to develop, but these are infrequent causes compared to cigarette smoking.
Risk Factors for Chronic Bronchitis
The major risk factor for individuals to develop chronic bronchitis are; Tobacco smoking and second-hand tobacco smoke exposure, repeated exposure to pollutants (especially airborne materials such as ammonia, sulfur dioxide, chlorine, bromine, hydrogen sulfide), dust, repeated attacks of acute bronchitis or pneumonia, and gastric reflux (by inhalation of gastric contents).
Pathophysiology
The disease is caused by an interaction between noxious inhaled agents and host factors, such as genetic predisposition or respiratory infections which cause injury or irritation to the respiratory epithelium of the walls and lumen of the bronchi and bronchioles. Chronic inflammation, edema, temporary bronchospasm, and increased production of mucus by goblet cells are the result. As a consequence, airflow into and out of the lungs is reduced, sometimes to a dramatic degree.
Most cases of chronic bronchitis are caused by smoking cigarettes or other tobacco products, although other examples of noxious agents include fumes from cleaning products and solvents, dust from occupational exposure, and air pollution. Ammonia, sulfur dioxide, chlorine, bromine, and hydrogen sulfide are especially harmful pollutants that are linked to respiratory diseases.
Chronic bronchitis must be distinguished from common allergies which also cause mucus hypersecretion and coughing fits. When chronic bronchitis progresses to include the pathologic changes of emphysema, it is often referred to as COPD.
Symptoms
- Bluish skin due to lack of oxygen (cyanosis).
- Breathing difficulties include wheezing and shortness of breath.
- Cough and sputum production are the most common symptoms; they usually last for at least 3 months and occur daily. The intensity of coughing and the amount and frequency of sputum production vary from patient to patient. Sputum may be clear, yellowish, greenish, or occasionally, blood-tinged.
- Fatigue.
- Fever may indicate a secondary viral or bacterial lung infection.
- Muscles around the ribs sink in as the child tries to breathe in (called intercostal retractions).
- An infant’s nostrils get wide when breathing
- Rapid breathing (tachypnea).
In addition, symptoms of sore throat, muscle aches, nasal congestion, and headaches can accompany the major symptoms. Severe coughing may cause chest pain.
Diagnosis
Medical history: It includes past and current smoking habits and living with someone who smokes, any history of on-the-job exposure to airborne irritants, and any family history of respiratory diseases, such as cystic fibrosis or emphysema.
Physical exam: Physical exam includes wheezes (high-pitched sounds that occur when air is pushed out through constricted airways), and rales (small rattling sounds that result when air moves through airways filled with fluid). The vibration from the chest percussion helps to determine the size and condition of the lungs.
- Complete blood cell count (CBC).
- Arterial blood gases (ABG) test.
- Chest X-ray.
- Spirometry.
- ECG.
Treatment
The goal of therapy for chronic bronchitis is to relieve symptoms, prevent complications and slow the progression of the disease. Quitting smoking is the most important and most successful treatment for chronic bronchitis, since continuing to use tobacco will only further damage the lungs.
Medications used for the treatment of bronchitis are:
Bronchodilator: Salmeterol, Albuterol, Metaproterenol, and Formoterol
Anticholinergic: Ipratropium bromide and Tiotropium
Steroids: Prednisone, Dexamethasone
PDE4 inhibitors: Roflumilast
Antibiotics: Macrolides, Azithromycin sulfonamides, Tetracyclines, Trimethoprim, and Fluoroquinolones
Vaccines: Patients with chronic bronchitis should receive a flu shot annually and pneumonia shot every five to seven years to prevent infections.
Oxygen Therapy: As a patient’s disease progresses, they may find it increasingly difficult to breathe on their own and may require supplemental oxygen.
Surgery: Lung volume reduction surgery, during which small wedges of damaged lung tissue are removed, may be recommended for some patients with chronic bronchitis.
Pulmonary Rehabilitation: An important part of chronic bronchitis treatment is pulmonary rehabilitation, which includes education, nutrition counseling, learning special breathing techniques, helping with quitting smoking, and starting an exercise regimen. Because people with chronic bronchitis are often physically uncomfortable, they may avoid any kind of physical activity. However, regular physical activity can actually improve a patient’s health and well-being.
Cough suppressants: Cough suppressants such as dextromethorphan may be helpful in reducing cough symptoms.
Prevention
The majority of instances of chronic bronchitis can be prevented by quitting smoking and avoiding second-hand smoke. Flu and pneumococcal vaccines can help to prevent repeated infections that may lead to the disease.
Certain industries (for example, chemical, textile, thermal, etc.) and farm workers are often associated with air-borne chemicals and dust; avoiding air-borne chemicals and dust with appropriate masks may prevent or reduce the individual’s chance of developing chronic bronchitis.
Good control of asthma may prevent chronic bronchitis from developing. The genetic predisposition to chronic bronchitis is not currently preventable.
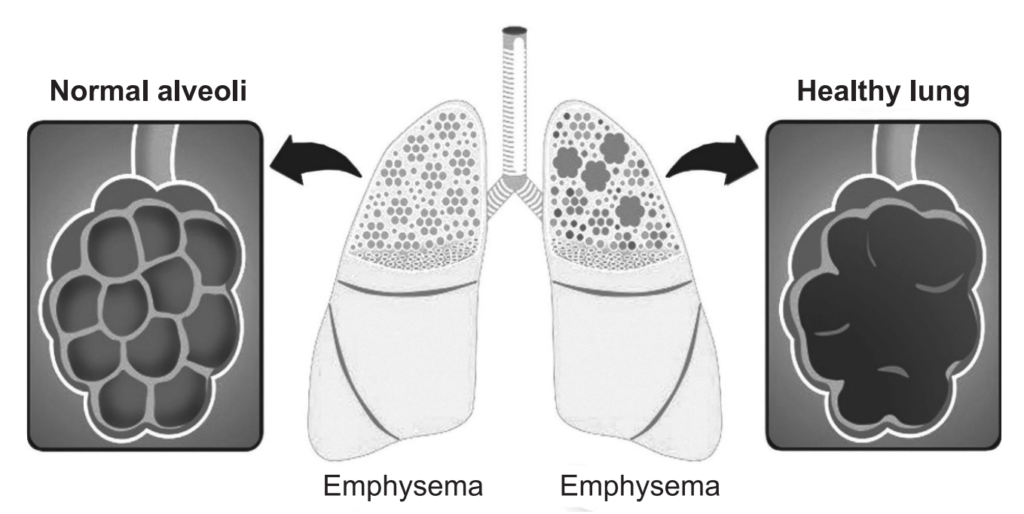
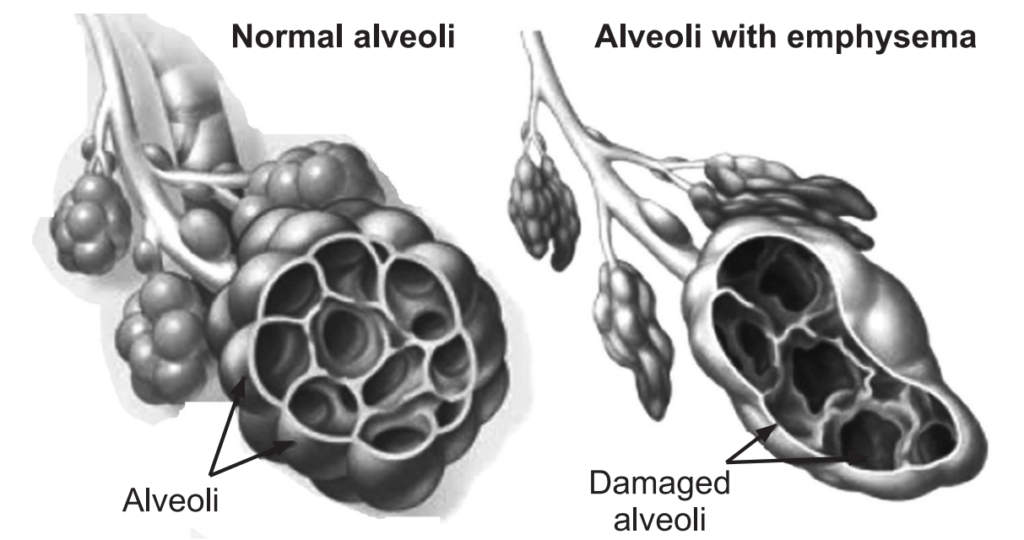
Emphysema
Emphysema is a long-term, progressive disease of the lungs that primarily causes shortness of breath due to over-inflation of the alveoli (air sacs in the lung). In people with emphysema, the lung tissues involved in the exchange of gases (oxygen and carbon dioxide) are impaired or destroyed. It is included in a group of diseases called chronic obstructive pulmonary disease or COPD. Emphysema is called an obstructive lung disease because the destruction of lung tissue around smaller airways (bronchioles), makes these airways unable to hold their shape properly when exhale. This makes them inefficient at transferring oxygen into the blood and taking carbon dioxide out of the blood.
Causes
The main cause of emphysema is long term exposure to airborne irritants, including:
- Tobacco smoke
- Marijuana smoke
- Air pollution
- Chemical fumes and dust
Cigarette smoking is by far the most dangerous behavior that causes people to develop emphysema, and it is also the most preventable cause. Other risk factors include a deficiency of an enzyme called α-1- antitrypsin, air pollution, airway reactivity, heredity, male sex, and age.
The importance of cigarette smoking as a risk factor for developing emphysema cannot be overemphasized. Cigarette smoke contributes to this disease process in two ways. It destroys lung tissue, which results in the obstruction of airflow, and it causes inflammation and irritation of airways that can add to airflow obstruction.
- Destruction of lung tissue occurs in several ways. First, cigarette smoke directly affects the cells in the airway responsible for clearing mucus and other secretions. Occasional smoking temporarily disrupts the sweeping action of tiny hairs called cilia that line the airways. Continued smoking leads to longer dysfunction of the cilia. Long-term exposure to cigarette smoke causes the cilia to disappear from the cells lining the air passages. Without the constant sweeping motion of the cilia, mucous secretions cannot be cleared from the lower respiratory tract. Furthermore, smoke causes mucous secretion to be increased, at the same time that the ability to clear the secretions is decreased. The resulting mucous deposition can provide bacteria and other organisms with a rich source of food and lead to infection.
- The immune cells in the lung, whose job is to prevent and fight infection, are also affected by cigarette smoke. They cannot fight bacteria as effectively, or clear the lungs of the many particles (such as tar) that cigarette smoke contains. In these ways, cigarette smoke sets the stage for frequent lung infections. Although these infections may not even be serious enough to require medical care, the inflammation caused by the immune system constantly attacking bacteria or tar leads to the release of destructive enzymes from the immune cells.
- Over time, enzymes released during this persistent inflammation lead to the loss of proteins responsible for keeping the lungs elastic. In addition, the tissue separating the air cells (alveoli) from one another also is destroyed. Over years of chronic exposure to cigarette smoke, the decreased elasticity and destruction of alveoli leads to the slow destruction of lung function.
- Air pollution acts in a similar manner to cigarette smoke. The pollutants cause inflammation in the airways, leading to lung tissue destruction.
- Close relatives of people with emphysema are more likely to develop the disease themselves. This is probably because the tissue sensitivity or response to smoke and other irritants may be inherited. The role of genetics in the development of emphysema, however, remains unclear.
- Abnormal airway reactivity, such as bronchial asthma, has been shown to be a risk factor for the development of emphysema.
- Men are more likely to develop emphysema than women. The exact reason for this is unknown, but differences between male and female hormones are suspected.
- Older age is a risk factor for emphysema. Lung function normally declines with age. Therefore, it is the reason that the older the person, the more likely they will have enough lung tissue destruction to produce emphysema.
Rarely, emphysema is caused by an inherited deficiency of a protein that protects the elastic structures in the lungs. It is called α-1-antitrypsin deficiency emphysema.
α-1-antitrypsin deficiency
α-1-antitrypsin (also known as α-1- antiprotease) AAT is a glycoprotein member of the serine protease inhibitor family that is synthesized in the liver and is secreted into the bloodstream. It is a substance that fights a destructive enzyme in the lungs called trypsin (or protease). Trypsin is a digestive enzyme, most often found in the digestive tract, where it is used to help the body digest food. It is also released by immune cells in their attempt to destroy bacteria and other material. People with an α-1-antitrypsin deficiency cannot fight the destructive effects of trypsin once it is released into the lung. The destruction of tissue by trypsin produces similar effects to those seen with cigarette smoking. The lung tissue is slowly destroyed, thus decreasing the ability of the lungs to perform appropriately. Foreign objects (e.g. bacteria) are trying to be destroyed but this enzyme destroys normal tissue since the second enzyme (antiprotease) responsible for controlling the first enzyme (protease) is not available or is poorly functioning. This is referred to as the “Dutch” hypothesis of emphysema formation.
The American Thoracic Society/ European Respiratory Society Guidelines recommend screening for AAT deficiency if emphysema is suspected in any patient younger than 45 years and with any of the following:
- Absence of recognized emphysema, risk factors such as smoking or occupational inhalational exposure. • Unexplained liver disease.
- Family history of AAT deficiency, COPD, bronchiectasis, or panniculitis.
- Positive c-ANCA (anti-neutrophilic cytoplasmic antibody) vasculitis.
- Unclear/idiopathic bronchiectasis.
- Asthma with persistent, fixed-airway obstruction despite therapy.
Risk Factors
Factors that increase the risk of developing emphysema include:
- Smoking: Emphysema is most likely to develop in cigarette smokers, but cigar and pipe smokers also are susceptible. The risk for all types of smokers increases with the number of years and amount of tobacco smoked.
- Age: The lung damage that occurs in emphysema develops gradually; most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60.
- Exposure to second-hand smoke: Second-hand smoke, also known as passive or environmental tobacco smoke, is smoke that you inadvertently inhale from someone else’s cigarette, pipe, or cigar. Being around second-hand smoke increases your risk of emphysema.
- Occupational exposure to fumes or dust: Breathe fumes from certain chemicals or dust from grain, cotton, wood, or mining products, are more likely to develop emphysema. This risk is even greater in cigarette smokers.
- Exposure to indoor and outdoor pollution: Breathing indoor pollutants, such as fumes from heating fuel, as well as outdoor pollutants, car exhaust, for instance, increases the risk of emphysema.
Symptoms
Two of the key symptoms of emphysema are shortness of breath and a chronic cough that appears in the early stages.
A person with shortness of breath, or dyspnea, feels being unable to catch a breath may start only during physical exertion, but as the disease progresses, it can start to happen during rest, too.
Emphysema and COPD develop over a number of years.
In the later stages, the person may have:
- Frequent lung infections,
- Excess production of mucus,
- Wheezing,
- Reduced appetite and weight loss,
- Fatigue,
- Blue-tinged lips or fingernail beds, or cyanosis, due to a lack of oxygen,
- Anxiety and depression,
- Sleep problems,
- Morning headaches due to a lack of oxygen, when breathing at night is difficult.
Complications
People who have emphysema are also more likely to develop:
- Collapsed lung (pneumothorax): A collapsed lung can be life-threatening in people who have severe emphysema because the function of their lungs is already so compromised. This is uncommon but serious when it occurs.
- Heart problems: Emphysema can increase the pressure in the arteries that connect the heart and lungs. This can cause a condition called cor pulmonale, in which a section of the heart expands and weakens.
- Large holes in the lungs: Some people with emphysema develop empty spaces in the lungs called bullae. They can be as large as half the lung. In addition to reducing the amount of space available for the lung to expand, giant bullae can increase your risk of pneumothorax.
Tests and Diagnosis
Diagnosis will carry out a physical examination and ask the patient about their symptoms and medical history. Some diagnostic tests may also be used, to confirm that the patient has emphysema rather than asthma and heart failure. If the patient has never smoked; a test may be carried out to see if the person has an α1- antitrypsin deficiency.
- A chest X-ray helps to identify changes in the lung that may indicate emphysema. The X-ray also may show the presence of an infection or a mass in the lung (such as a tumor) that could explain symptoms. Shortness of breath has many causes. The chest X-ray is considered to be the quickest and easiest test to begin to separate the different possible causes and formulate a diagnosis.
- Lung function tests can give specific information about how the lungs work mechanically. In these tests, the patient has to breathe into a tube that is connected to a computer or some other monitoring device, which can record the necessary information. The tests measure how much air in the lungs can hold, how quickly lungs can expel air during expiration, and how much reserve capacity of lungs have for increased demand, such as during exercise.
- The blood test is used to detect a family history of α1-antitrypsin deficiency to evaluate genetic disease.
- Blood tests may also be used to check white blood cell count, which can sometimes indicate an acute infection. This information can be used with the chest X-ray to evaluate for pneumonia, bronchitis, or other respiratory infections that can make emphysema worse.
- Another blood test that may be helpful, especially in the hospital setting, is called arterial blood gas. This test helps determine how much oxygen and carbon dioxide are in the blood.
Treatment
Treatment for emphysema can take many forms in a step-wise approach, depending on the severity of the condition. Medications used for the treatment of emphysema are:
Bronchodilator: Salmeterol, Albuterol, Metaproterenol, and Formoterol
Anticholinergic: Ipratropium bromide and Tiotropium
Steroids: Prednisone, Dexamethasone
PDE4 inhibitors: Roflumilast
Stop smoking: This recommendation for people with emphysema, quitting smoking may halt the progression of the disease and improve the function of the lungs to some extent. Lung function deteriorates with age. In those susceptible to developing COPD, smoking can result in a five-fold deterioration of lung function. Smoking cessation may return lung function from this rapid deterioration to its normal rate after smoking is stopped.
Antibiotics: These medications are often prescribed for people with emphysema who have increased shortness of breath. Even when the chest X-ray does not show pneumonia or evidence of infection, people treated with antibiotics tend to have shorter episodes of shortness of breath. It is suspected that infection may play a role in an acute bout of emphysema, even before the infection worsens into pneumonia or acute bronchitis.
Oxygen Therapy: As patients’ disease progresses, they may find it increasingly difficult to breathe on their own and may require supplemental oxygen.
Surgery: People with severe emphysema sometimes undergo surgery to reduce lung volume or carry out lung transplantation. Lung volume reduction surgery removes small wedges of the damaged, emphysematous, lung tissue. This is thought to enhance lung recoil and improve the function of the diaphragm. In severe cases, this can improve lung function, exercise tolerance, and quality of life.
Lung transplantation improves the quality of life, but not life expectancy, for people with severe emphysema. Lifelong drug therapy is necessary to prevent the immune system from rejecting the new tissue. One or both lungs may be transplanted.
Make sure you also check our other amazing Article on: Asthma