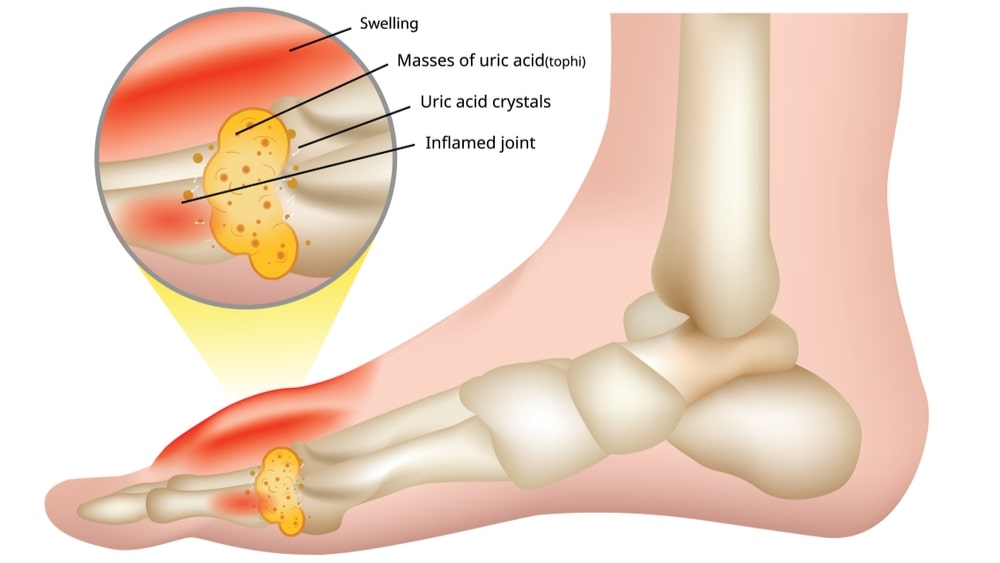
Gout is a metabolic disorder characterized by elevated serum uric acid levels and deposits of urate crystals in synovial fluids and surrounding tissues in joints. It is a type of arthritis that is characterized by sudden, severe attacks of joint pain with redness, warmth, and swelling in the affected area. It usually attacks only one joint at a time. It most often strikes the joint of the big toe, which is also known as podagra, but other toes can also be involved.
Table of Contents
Epidemiology
Gout affects around 1–2% of the Western population at some point in their lifetimes and is becoming more common. Rates of gout have approximately doubled between 1990 and 2010. This rise is believed due to increasing life expectancy, changes in diet, and an increase in diseases associated with gouts, such as metabolic syndrome and high blood pressure. A number of factors have been found to influence rates of gout, including age, race, and the season of the year. In men over the age of 30 and women over the age of 50, the prevalence is 2%.
Some studies have found that attacks of gout occur more frequently in the spring. This has been attributed to seasonal changes in diet, alcohol consumption, physical activity, and temperature.
Causes
Gout is caused initially by an excess of uric acid in the blood (hyperuricemia). Uric acid is produced in the body through the breakdown of purines-specific chemical compounds that are found in certain foods such as meat, poultry, and seafood.
Normally, uric acid dissolves in the blood and is excreted from the body in urine via the kidneys. If too much uric acid is produced or not enough is excreted then it can build up and form the needle-like crystals that cause inflammation and pain in the joints and surrounding tissue.
There are a number of factors that can increase the likelihood of hyperuricemia, and therefore gout:
Age and gender: Men produce more uric acid than women. But after menopause, the uric acid level in women is equal to men.
Genetics: A family history of gout increases the likelihood of the condition developing.
Lifestyle Factors: Alcohol consumption interferes with the removal of uric acid from the body. Eating a high-purine diet also increases the amount of uric acid in the body.
Lead exposure: Chronic lead exposure has been linked in some cases to gout.
Medications: Certain medications can increase the levels of uric acid in the body, such as diuretics and drugs containing salicylate, Niacin, etc.
Weight: Being overweight increases the risk as there is more tissue in the body for turnover or breakdown, leading to the production of excess uric acid.
Other health problems: If the kidneys are unable to eliminate waste products adequately (renal insufficiency) then uric acid levels can remain high. Other conditions that can contribute are high blood pressure (hypertension), diabetes, and hypothyroidism.
People with Kelley-Seegmiller syndrome or Lesch-Nyhan syndrome have a partial or complete deficiency in an enzyme that helps to control uric acid levels.
Pathophysiology
Gout is a disorder of purine metabolism and occurs when its final metabolite, uric acid, crystallizes in the form of monosodium urate, precipitating in joints, on tendons, and in the surrounding tissues. These crystals then trigger a local immune-mediated inflammatory reaction, with one of the key proteins in the inflammatory cascade being interleukin. An evolutionary loss of uricase, which breaks down uric acid, in humans and higher primates has made this condition common.
The triggers for the precipitation of uric acid are not well understood. While it may crystallize at normal levels, it is more likely to do so as levels increase. Other factors believed important in triggering an acute episode of arthritis include cool temperature, rapid changes in uric acid levels, acidosis, articular hydration, and extracellular matrix proteins such as proteoglycans, collagens, and chondroitin sulfate.
Rapid changes in uric acid may occur due to a number of factors, including trauma, surgery, chemotherapy, diuretics, and stopping or starting allopurinol. Calcium channel blockers are associated with a lower risk of gout as compared to other medications for hypertension.
Clinical Manifestations
The signs and symptoms of gout are almost always acute, occurring suddenly often at night, and without warning.
Intense joint pain: Gout usually affects the large joint of the big toe, but it can occur in the feet, ankles, knees, hands, and wrists. The pain is likely to be most severe within the first 12 to 24 hours after it begins.
Lingering discomfort: After the most severe pain subsides, some joint discomfort may last from a few days to a few weeks. Later attacks are likely to last longer and affect more joints.
Inflammation and redness: The affected joint or joints become swollen, tender, and red.
Complications
People with gout can develop more severe conditions, such as:
Recurrent gout: Some people may never experience gout signs and symptoms again. But others may experience gout several times each year. Medications may help prevent gout attacks in people with recurrent gout.
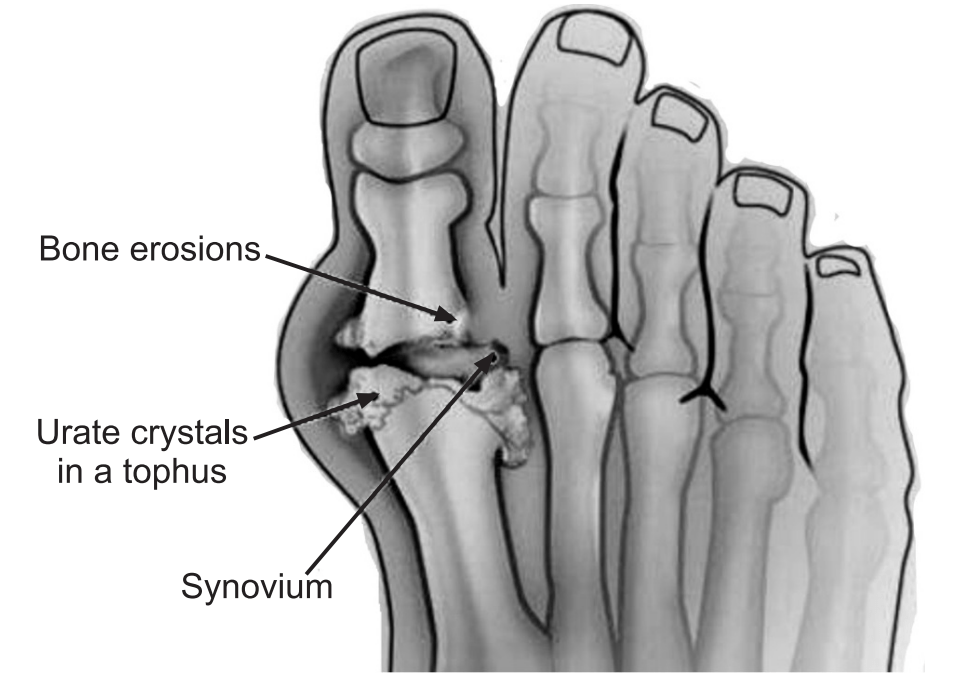
Advanced gout: Untreated gout may cause deposits of urate crystals to form under the skin in nodules called tophi. Tophi can develop in several areas such as fingers, hands, feet, elbows, or Achilles tendons along the back of the ankle. Tophi usually are not painful, but they can become swollen and tender during gout attacks.
Kidney stones: Urate crystals may collect in the urinary tract of people with gout, causing kidney stones.
Symptoms
Symptoms of gout include severe pain, bone erosion, redness, and swelling in joints, often the big toe.
Diagnosis
Joint fluid test: Joint fluid test (arthrocentesis) is useful to see whether uric acid crystals are present. This is the only test for the diagnosis of gout.
Blood test: To measure the uric acid level in the blood. Blood test results can be misleading, although some people have high uric acid levels, and never experience gout. And some people have signs and symptoms of gout but do not have unusual levels of uric acid in their blood.
Urine Test: A test to measure levels of uric acid in urine.
X-ray: X-rays of extremities (hands and feet) are sometimes useful in the late stages of the disease; X-rays are not usually helpful in the early diagnosis. Pain often causes people to seek medical attention before any long-term changes can be seen on an X-ray. But X-rays may help to rule out other causes of arthritis.
Treatment
The goals of treatment for gout are fast pain relief and prevention of future gout attacks and long-term complications, such as joint destruction and kidney damage.
NSAIDs: NSAIDs may control inflammation and pain in people with gout. NSAIDs include indomethacin, ibuprofen, naproxen, and etoricoxib.
Colchicine: A type of pain reliever that effectively reduces gout pain, especially when started soon after symptoms appear.
Corticosteroids: Corticosteroid medications, such as the drug prednisone, may control gout inflammation and pain. Corticosteroids may be administered in pill form, or they can be injected into the joint. Corticosteroids are generally reserved for people who cannot take either NSAIDs or colchicine.
Medications that block uric acid production: Xanthine oxidase inhibitors, including allopurinol and febuxostat, limit the amount of uric acid that the body makes.
This may lower blood uric acid levels and reduce the risk of gout. Side effects of allopurinol include a rash and low blood counts. Febuxostat side effects include rash, nausea, and reduced liver function.
If gout symptoms have occurred OFF and ON without treatment for more than 10 years, uric acid crystals may have built up in the joints to form gritty, chalky nodules called tophi. If tophi are causing infection, pain, pressure, and deformed joints, treatment includes Xanthine oxidase inhibitors, which may shrink the tophi until they disappear.
Medication that improves uric acid removal: Probenecid improves the kidney’s ability to remove uric acid from the body. This may lower uric acid levels and reduce the risk of gout, but the level of uric acid in urine is increased.
Pegloticase: This medicine is for gout that has lasted a long time and has not responded to other treatments.
Prevention
During symptom-free periods, these dietary guidelines may help protect against future gout attacks.
Drink 8 to 16 cups (about 2 to 4 liters) of fluid each day, with at least half being water. Eat a moderate amount of protein, preferably from healthy sources, such as low-fat or fat-free dairy, eggs, and nut butter.
Limit daily intake of meat, fish, and poultry to 4 to 6 ounces (113 to 170 grams). Maintain desirable body weight.
Make sure you also check our other amazing Article on: Osteoporosis