Typhoid fever is also called enteric fever. It is an acute infectious illness associated with fever that is most often caused by the Salmonella typhi bacteria. It can also be caused by Salmonella paratyphi, a related bacterium that usually leads to a less severe illness. The bacteria are deposited through fecal contamination in water or food by a human carrier and are then spread to other people in the area. Typhoid fever is rare in industrial countries but continues to be a significant public health issue in developing countries.
Table of Contents
Pathophysiology
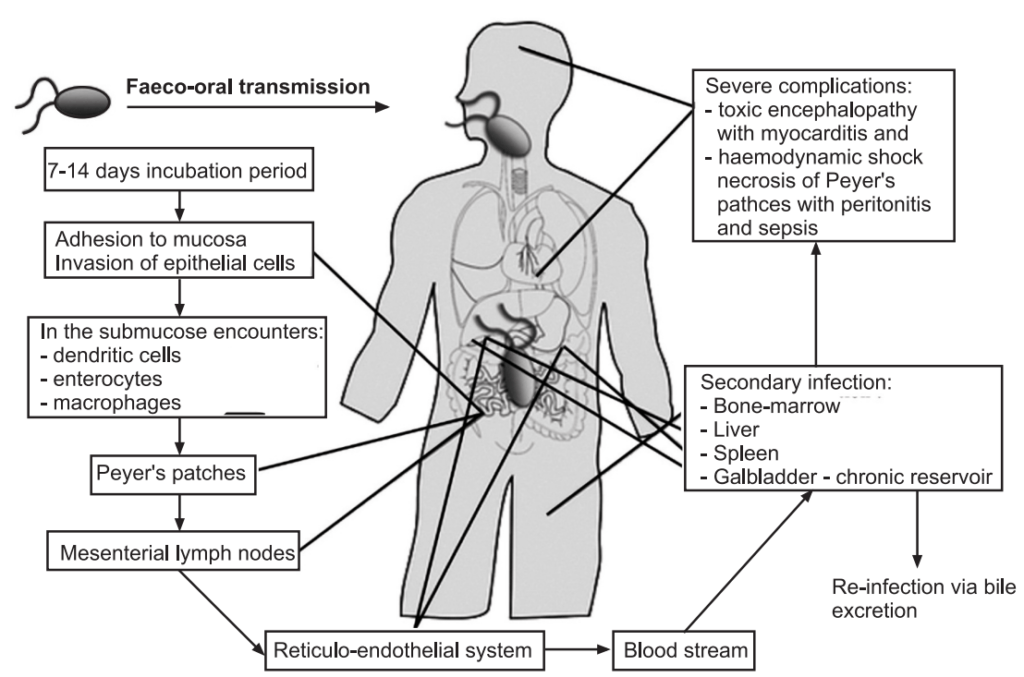
All the pathogenic Salmonella species, when present in the gut are engulfed by phagocytic cells, which then pass them through the mucosa and present them to the macrophages in the lamina proprietor. Nontyphoidal salmonellae are phagocytized throughout the distal ileum and colon. With toll-like receptor (TLR)–5 and TLR[1]4/MD2/CD-14 complex, macrophages recognize pathogen-associated molecular patterns (PAMPs) such as flagella and lipopolysaccharides. Macrophages and intestinal epithelial cells then attract T cells and neutrophils with interleukin 8 (IL-8), causing inflammation and suppressing the infection.
In contrast to the nontyphoidal salmonellae, S typhi and paratyphi enter the host’s system primarily through the distal ileum. They have specialized fimbriae that adhere to the epithelium over clusters of lymphoid tissue in the ileum (Peyer patches), the main relay point for macrophages traveling from the gut into the lymphatic system. The bacteria then induce their host macrophages to attract more macrophages.
S typhi has a VI capsular antigen that masks PAMPs, avoiding neutrophil-based inflammation, while the most common paratyphi Serova, paratyphi A, does not. This may explain the greater infectivity of typhi compared with most of its cousins.
Typhoidal salmonella co-opts the macrophages’ cellular machinery for their own reproduction as they are carried through the mesenteric lymph nodes to the thoracic duct and the lymphatics and then through to the reticuloendothelial tissues of the liver, spleen, bone marrow, and lymph nodes. Once there, they pause and continue to multiply until some critical density is reached. Afterward, the bacteria induce macrophage apoptosis, breaking out into the bloodstream to invade the rest of the body.
The bacteria then infect the gallbladder via either bacteremia or direct extension of infected bile. The result is that the organism re-enters the gastrointestinal tract in the bile and reinfects Peyer patches. Bacteria that do not reinfect the host are typically shed in the stool and are then available to infect other hosts.
Epidemiology
Typhoid fever occurs worldwide, primarily in developing nations whose sanitary conditions are poor. Typhoid fever is endemic in Asia, Africa, Latin America, the Caribbean, and Oceania, but 80% of cases come from Bangladesh, China, India, Indonesia, Laos, Nepal, Pakistan, or Vietnam. Within those countries, typhoid fever is most common in underdeveloped areas. Typhoid fever infects roughly 21.6 million people (incidence of 3.6 per 1,000 population) and kills an estimated 200,000 people every year. In the United States, most cases of typhoid fever arise in international travelers. The average yearly incidence of typhoid fever per million travelers from 1999 to 2006 by country or region of departure was as follows:
- Canada – 0
- Western hemisphere outside Canada / United States – 1.3
- Africa – 7.6
- Asia – 10.5
- India – 89 (122 in 2006)
- Total (for all countries except Canada/United States) – 2.2
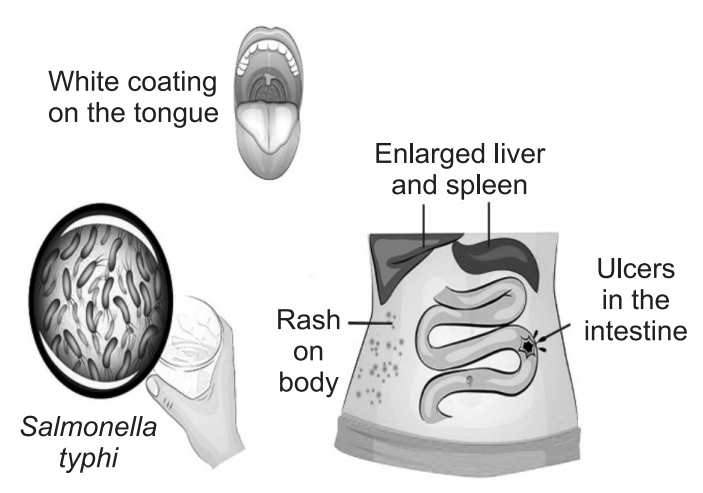
Symptoms and Complications
Symptoms usually appear 1 or 2 weeks after infection but may take as long as 3 weeks to appear. Typhoid usually causes a high, sustained fever, often as high as 40°C (104°F), and extreme exhaustion.
Other common symptoms include:
- Constipation,
- Cough,
- Headache,
- Loss of appetite,
- Stomach pains,
- Sore throat.
Rarer symptoms include:
- Bleeding from the rectum,
- Delirium,
- Diarrhea.
Temporary pink spots on the chest and abdomen
Diagnosis
Infection with typhoid or paratyphoid fever results in low-grade septicemia. It is diagnosed as follows:
Differential Diagnosis:
The group of symptoms that most clearly suggests the diagnosis of typhoid fever is:
- Gradually increasing fever with evening exacerbation and morning remission.
- General malaise with the headache.
- Furred tongue with red edges and tip.
- Epistaxis.
- Relatively slow pulse (possibly dicrotic).
- Abdominal distension with increased bowel sounds.
- Tenderness in the right iliac fossa on firm pressure.
- A roseolar eruption is confined principally to the abdomen and chest.
- Splenomegaly.
- Bronchial catarrh.
The differential diagnosis of this group of symptoms will depend on travel history and may include a wide variety of tropical and non-tropical causes of fever and rash. Always consider co-existent malaria or schistosomiasis and others.
Organism Culture:
- Diagnosis is made by culturing the organism. This may be obtained from stool or other sources.
- Blood cultures are only positive in 40- 60% of cases. However, this may be enhanced to above 80% using two sets of blood cultures and modern methods.
- The most sensitive source (90% isolation rate) is bone marrow aspiration.
- Isolation of S. Typhi is highest in the first week and becomes more difficult as time passes.
Serology:
- The traditional serological test is Widal’s test. It measures agglutinating antibodies against flagellar (H) and somatic (O) antigens of S. Typhi.
- High or rising O antibody titers generally indicate acute infection, whereas H antibody is used to identify the type of infection.
- The test is positive on admission in between 40-60% of patients but the test has an enormous variation between laboratories in terms of sensitivity, specificity, and predictive value.
- The validity of rapid diagnostic tests for typhoid and paratyphoid was submitted for Cochrane review in 2010.
Treatment
Typhoid fever is treated with antibiotics that kill the Salmonella bacteria. Prior to the use of antibiotics, the fatality rate was 20%. The death occurred from overwhelming infection, pneumonia, intestinal bleeding, or intestinal perforation. With antibiotics and supportive care, mortality has been reduced to 1%-2%. With appropriate antibiotic therapy, there is usually improvement within one to two days and recovery within seven to 10 days. Several antibiotics are effective for the treatment of typhoid fever.
- Chloramphenicol was the original drug of choice for many years. Because of rare serious side effects, chloramphenicol has been replaced by other effective antibiotics.
- Fluoroquinolones like Ciprofloxacin, Gatifloxacin, and Ofloxacin are the most frequently used drugs for nonpregnant patients.
- Ceftriaxone an intramuscular injection medication is an alternative for pregnant patients.
- Ampicillin and trimethoprim-sulfamethoxazole are frequently prescribed antibiotics although resistance has been reported in recent years.
- Antipyretic therapy is used if required.
- Steroids have occasionally been used in severe cases. However, they may induce relapse, so are not generally recommended.
- Surgical – if perforation of the bowel occurs, it will require closure. Treatment with antibiotics alone was once favored but simple closure and drainage are required.
Complications
- The two most common complications are hemorrhage (including disseminated intravascular coagulation) and perforation of the bowel. Before antibiotics, perforation had a mortality of around 75%.
- Jaundice may be due to hepatitis, cholangitis, cholecystitis, or hemolysis.
- Pancreatitis with acute kidney injury and hepatitis with hepatomegaly are rare.
- Toxic myocarditis occurs in 1-5% of patients (ECG changes may be present). It is a significant cause of death in endemic areas.
- Toxic confusional states and other neurological and psychiatric disturbances have been reported.
Prevention
- Wash hands thoroughly with soap and water after going to the toilet and before eating.
- Boil or disinfect all water before drinking it – use disinfectant tablets or liquid available in pharmacies or drink commercially bottled (preferably carbonated) beverages.
- Peel all fruit and vegetable skins before eating.
- Keep flies away from food.
- Watch out for ice cubes, ice cream, and unpasteurized milk, which can easily be contaminated.
- Cook all food thoroughly and eat it while it is hot.
- Be aware of the “danger foods” shellfish, salads, and raw fruit and vegetables.
- Do not eat food or drink beverages from street vendors.
Make sure you also check our other amazing Article on: Gout
