Anatomy and physiology of the Liver
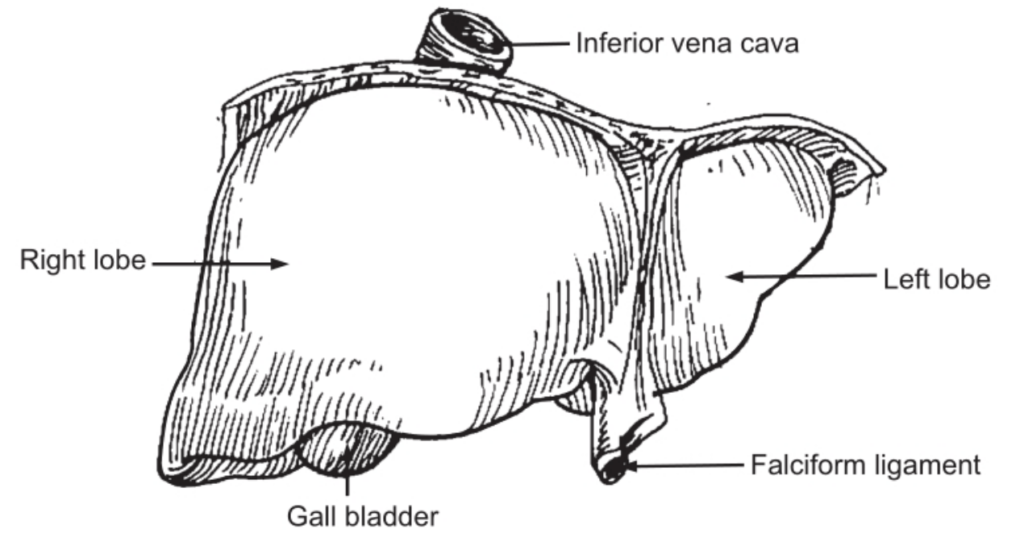
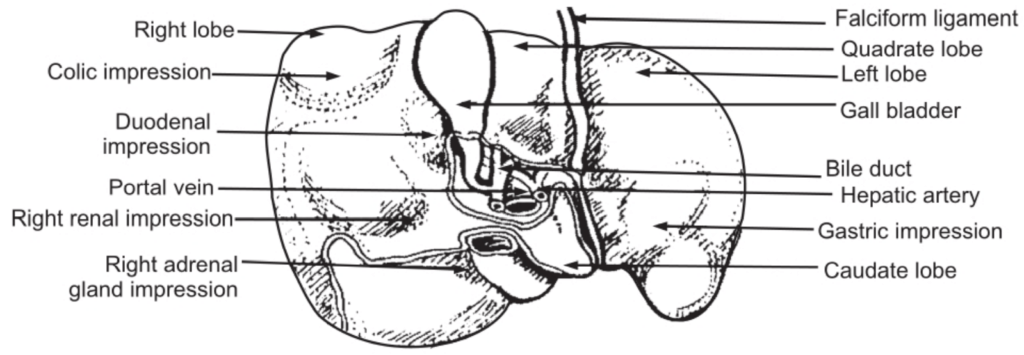
The liver is the largest gland in the body situated in the uppermost part of the abdominal cavity on the right side beneath the diaphragm. It weighs about 1500 grams and is irregular in shape. The upper surface is convex and lies beneath the diaphragm, while the under surface is irregular and is in contact with the stomach, duodenum, right colic flexure of the colon, and right kidney. It is enclosed in a thin capsule and partially covered by a layer of peritoneum. It is divided mainly into two lobes the right and left, however, the under the surface of the liver shows two more lobes; the quadrate lobe is the quadrilateral area between the gall bladder and the fosse for the round ligament, and the caudate lobe is another quadrilateral area between inferior vena cava and the fosse for ligament venosum.
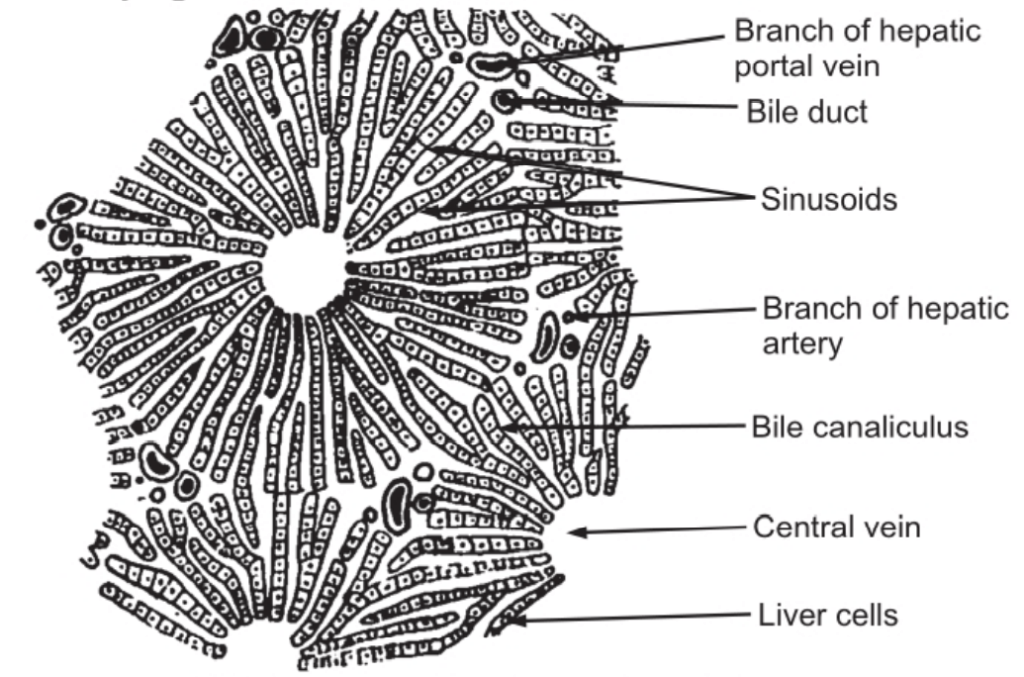
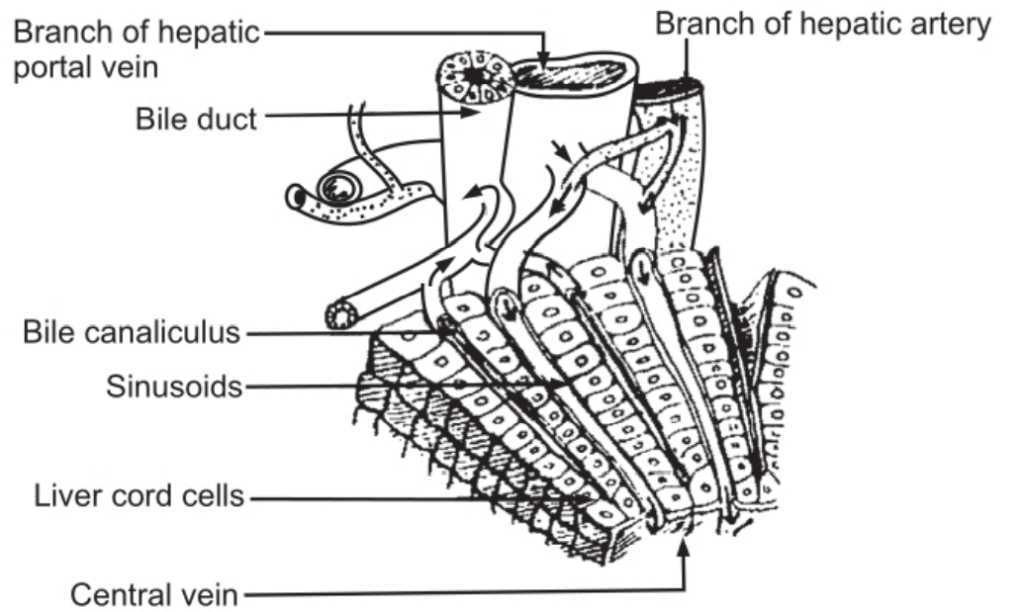
The liver is made up of lobules which are polyhedral in shape. Each lobule is composed of cubical cells arranged radially, radiating from the central vein. Between two columns of cells, there are sinusoids containing a mixture of blood from the tiny branches of the portal vein and the hepatic artery. Masses of such cells which form hepatic lobule (01 mm diameter) are separated from one another by connective tissue. Branches of the portal vein, hepatic artery, and bile duct are enclosed in a tissue covering called as the ‘Gilson’s capsule’ which forms the portal canal.
Such portal canals are present surrounding the lobules. The blood from sinusoids comes in close contact with the liver cells. The sinusoids pour the blood into the vein in the center of the lobule called as the interlobular vein. Interlobular veins from different lobules unite to form sublobular veins which in turn unite to form hepatic veins passing directly into the inferior vena cava. Bile is formed by the hepatic cells and is secreted into the fine bile canaliculi which commence between the columns of liver cells and carry bile to the periphery of the hepatic lobule. The bile canaliculi join up to form larger bile canals until eventually they form the right and left hepatic ducts which drain bile from the liver. Thus, as shown in Fig. 1.1 (b) there is an alternate arrangement of sinusoids (carrying blood) and bile canaliculi (carrying bile) in a lobule.
Large bile ducts have a lining of columnar epithelium and outer fibrous muscular tissue. By means of contraction of the muscular layer, bile is carried away. It is temporarily stored in the gall bladder.
Physiology of Liver
Secretion of bile
Hepatic cells secrete an alkaline fluid called bile. It is composed of 90 percent water, bile salts (sodium glycocholate, sodium taurocholate), bile pigments (bilirubin, biliverdin), cholesterol, and mucin. Bile salts are helpful in the digestion and absorption of fats. They reduce the surface tension of fats and help in their emulsification. RBCs are destroyed in the liver and spleen. The hemoglobin of RBCs is broken down into globin and haem. Haem is again broken down into iron and porphyrins, which form bile pigments later on.
Glycogenic functions
The portal vein carries the blood from the digestive tract which contains glucose and amino acids. It pours the blood into the liver. The hepatic cells, by the action of enzymes, convert glucose into glycogen and it is then stored in the liver. Whenever there is a need for energy in the body, the hepatic cells convert glycogen to glucose and pass it to the body cells through blood circulation. Thus, this glycogenic function helps to maintain the sugar level constant in the blood.
Formation of urea
The portal vein carries blood containing amino acids to the liver. Hepatic cells by the action of their enzymes cause deamination of amino acids, i.e. amino group is set free which forms urea. Urea is carried away to the kidneys by the blood and is given out of the body through urine.
Denaturation of fats
The digested fats in the form of the fatty acids and glycerol are absorbed in the central lacteal duct. The fatty acids and glycerol again unite to form fats. This fat is carried away by the blood and is stored in the different tissues in saturated form. Whenever the energy is needed, this saturated stored fat is carried to the liver by blood. Then the hepatic cells cause the desaturation of this fat and pass to different tissues for utilization.
Functions related to blood
- Formation of RBCs in fetal life.
- Destruction of RBCs forming bile pigments and iron.
- Formation of plasma proteins, i.e. albumin and globulin.
- Formation of prothrombin and fibrinogen responsible for blood clotting.
- Formation of heparin, a natural anticoagulant in the blood.
- Storage of iron, vitamin B12.
Maintenance of body temperature
The numerous chemical reactions occur in the liver, heat is generated which is helpful in maintaining body temperature.
Excretion of toxic substances
The toxic substances entering the body through the alimentary canal are destroyed in the liver, e.g. alcohol, some drugs, etc.
As the liver is responsible for a number of intermediate metabolic reactions, it is called the chemical factory in the body.
Make sure you also check our other amazing Article on: Spinal Cord