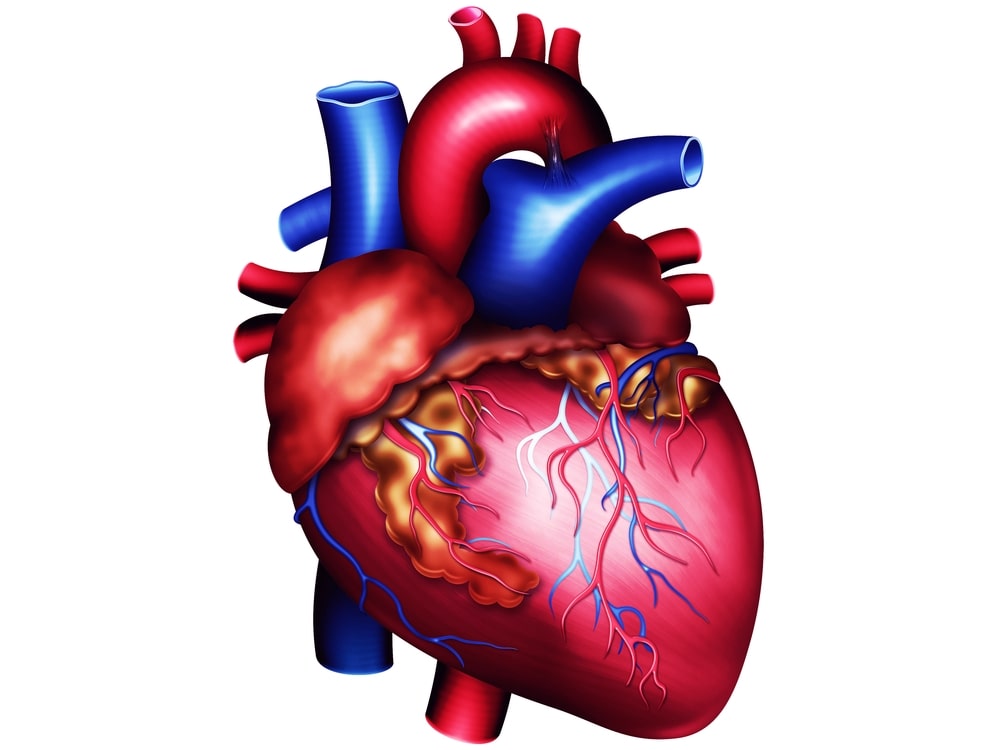
Anatomy of The heart is a roughly cone-shaped hollow muscular organ. It is about 10 cm long and is of the size of a person’s fist. It weighs about 300 grams in an adult.
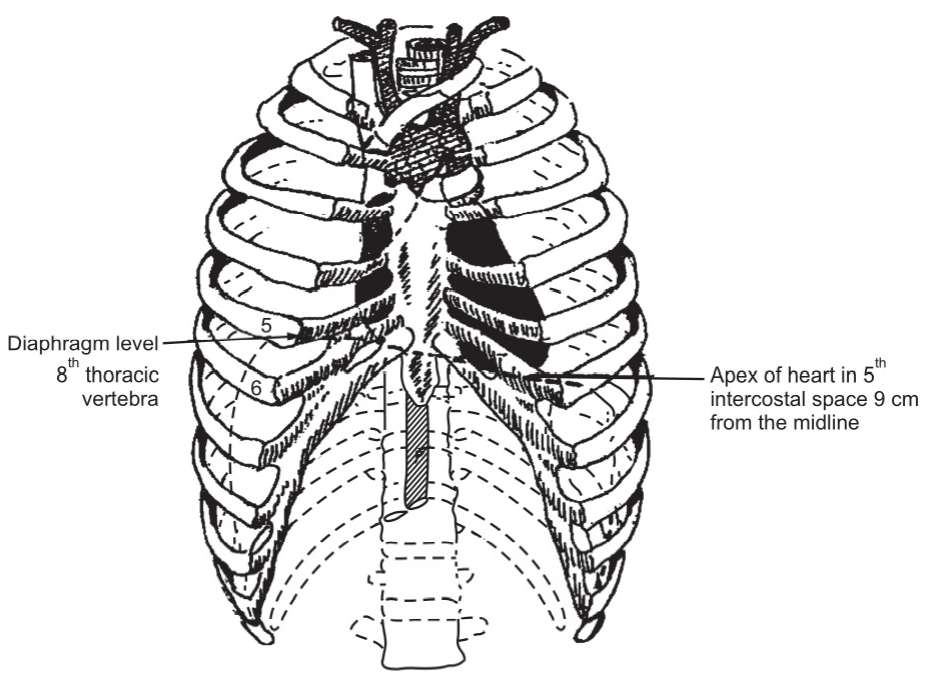
It is located in the thoracic cavity in the mediastinum between the lungs. It lies obliquely, a little more to the left than the right, and presents a base above, and an apex below. It is about 12 cm long, 09 cm wide at its broadest point, and 06 cm thick.
The apex is about 09 cm to the left of the midline at the level of the fifth intercostal space; the base extends to the level of the second rib.
Following organs are associated with the heart:
Inferiorly: The apex rests on the central tendon of the diaphragm.
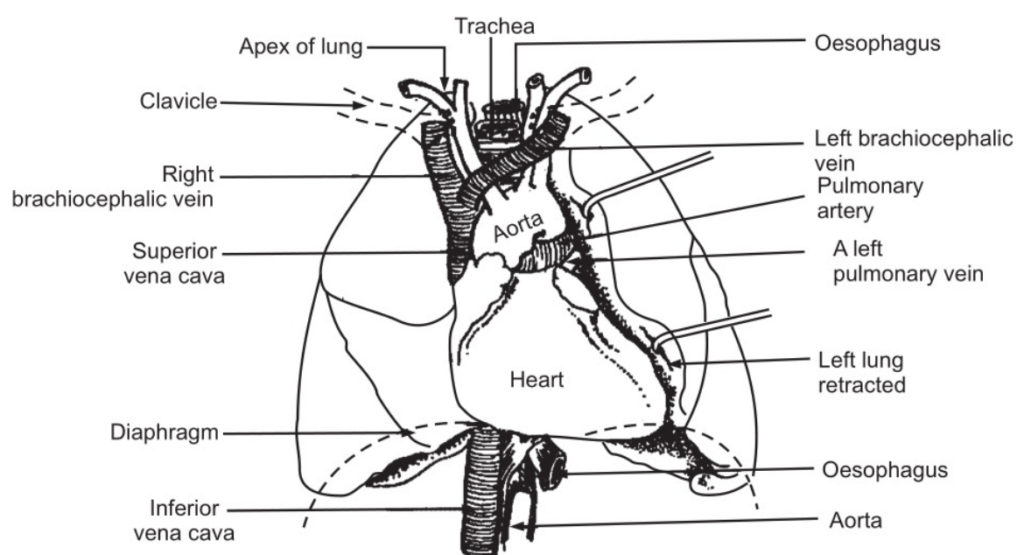
Superiorly: The great blood vessels, i.e. the aorta, superior vena cava, pulmonary artery, and pulmonary veins.
Posteriorly: The oesophagus, trachea, left and right bronchus, descending aorta, inferior vena cava, and thoracic vertebrae.
Laterally: The lungs; the left lung overlaps the left side of the heart.
Anteriorly: The sternum, ribs, and intercostal muscles.
Table of Contents
Structure of the Heart
The heart is composed of three layers of tissue: pericardium, myocardium, and endocardium.
Pericardium
It is made up of two sacs. The outer sac consists of fibrous tissue and the inner of a double layer of serous membrane. The outer fibrous sac is continuous with the tunica adventitia of the great blood vessels above and is adherent to the diaphragm below. Its fibrous nature prevents over-distension of the heart. The serous membrane consists of flattened epithelial cells. It secretes serous fluid into the space between the visceral and parietal layers which allows smooth movement between them when the heartbeats. The space between the parietal and visceral pericardium is only a potential space.
Myocardium
It is composed of specialized cardiac muscle tissue found only in the heart. It is formed with the help of cardiac fibers. Each fiber has a nucleus and one or more branches. The ends of the cells and their branches are in close contact with the ends and branches of adjacent cells. Microscopically these joints or intercalated discs are observed as thicker, darker lines.
This arrangement gives the cardiac muscle appearance of being a sheet of muscle rather than a large number of individual cells. When an impulse is initiated it spreads from cell to cell via the branches and intercalated discs over the whole sheet of muscle, causing contraction. For this reason, the heart is termed as a ‘functional syncytial’. The myocardium is thickest at the apex and thins out towards the base. It is the thickest in the left ventricle. The atria and ventricles are separated by a ring of fibrous tissue. When a wave of electrical activity passes over the atrial muscle, it can only spread to the ventricles through the conductive system which extends across the fibrous ring from atria to ventricles.
Endocardium
It forms the lining of the myocardium and the heart valves. It is a thin, smooth, glistening membrane which permits a smooth flow of blood inside the heart. It consists of epithelial cells, continuous with the endothelium that lines the blood vessels.
INTERIOR OF THE HEART
The heart is divided into a right and left side by a partition consisting of myocardium covered by endocardium. Each side is divided by an atrioventricular valve into an upper chamber, the atrium, and a lower chamber, the ventricle. The atrioventricular valves are formed by double folds of the endocardium strengthened by a little fibrous tissue. The right atrioventricular valve (tricuspid valve) has three flaps or cusps and the left atrioventricular valve (mitral valve) has two cusps. The valves, between the atria and ventricles, open and close passively according to changes in pressure in the chambers. They open when the pressure in the atria is greater than that in the ventricles. During ventricular systole (contraction) the pressure in the ventricles rises above that in the atria and the valves shut for a short while preventing backflow of blood. The valves are prevented from opening upwards into the atria by tendinous cords, chordae tendineae, which extend from the inferior surface of the cusps to little projections of myocardium covered with endothelium, called papillary muscles.
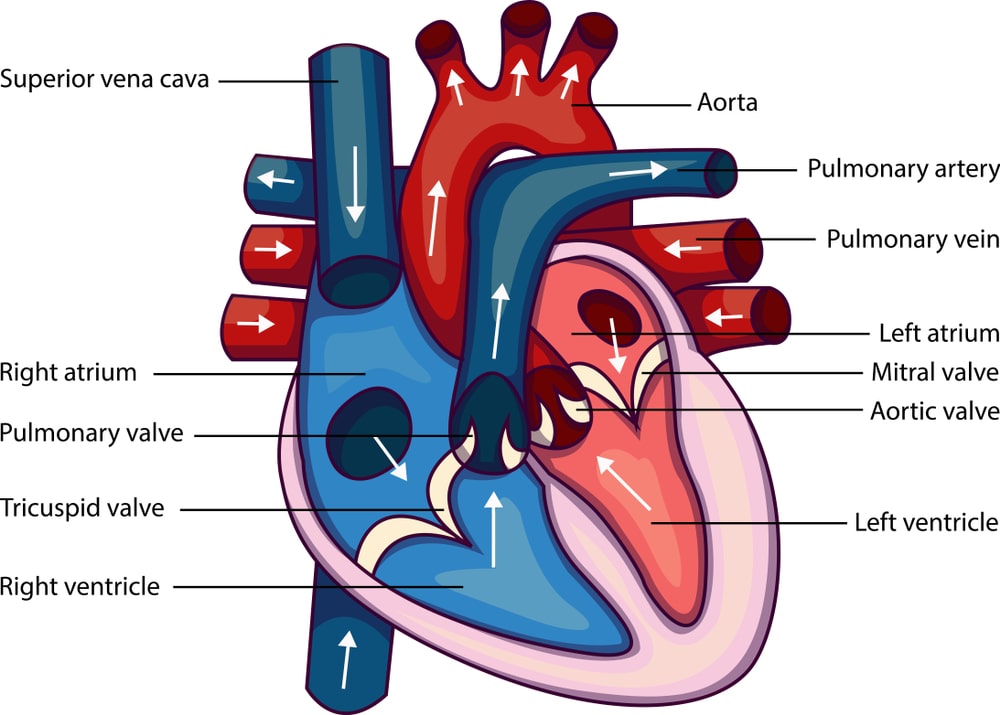
FLOW OF THE BLOOD THROUGH THE HEART
The superior and inferior venae cavae are the two largest veins in the body. They empty their contents into the right atrium. This blood passes through the right atrioventricular valve into the right ventricle, and from there it is pumped into the pulmonary artery, which carries deoxygenated blood to the lungs. The opening of the pulmonary artery is controlled by the pulmonary valve, formed by three semi lunar cusps. This valve prevents the back flow of blood into the right ventricle when the ventricle muscle relaxes. The pulmonary artery then divides into left and right pulmonary arteries which carry the venous blood to the lungs where it gets purified.
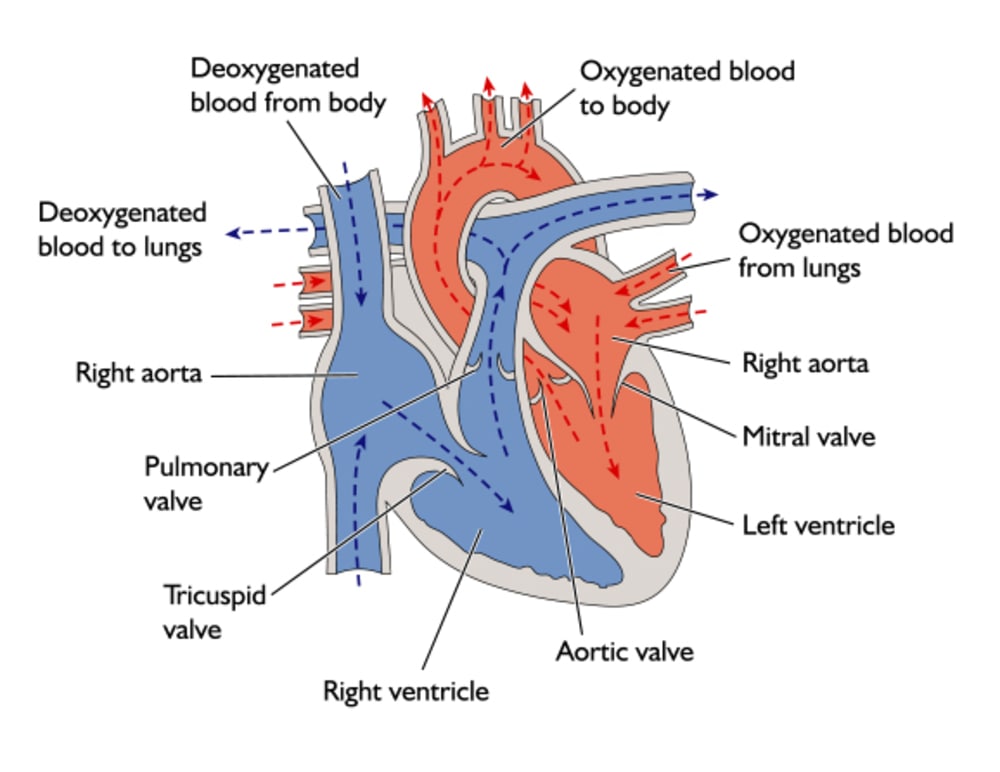
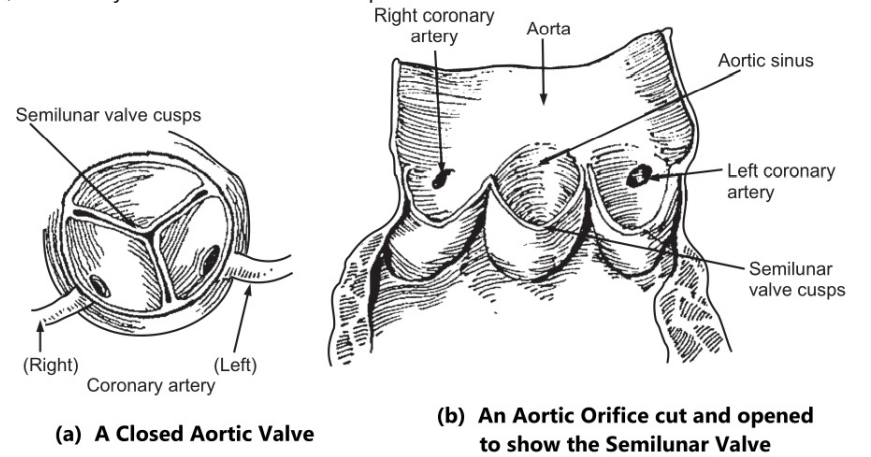
Two pulmonary veins from each lung carry oxygenated blood to the left atrium. Then it passes through the left atrioventricular valve into the left ventricle, from where it is pumped into the aorta for general circulation. The opening of the aorta is controlled by the aortic valve, formed by the three semilunar cusps.
It is to be noted that both atria contract at the same time and this is followed by the simultaneous contraction of both ventricles. The muscle layer of the walls of the atria is very thin in comparison with that of the ventricles. The muscle layer is the thickest in the wall of the left ventricle. The pulmonary trunk leaves the heart from the upper part of the right ventricle, and the aorta leaves from the upper part of the left ventricle.
BLOOD SUPPLIED TO THE HEART
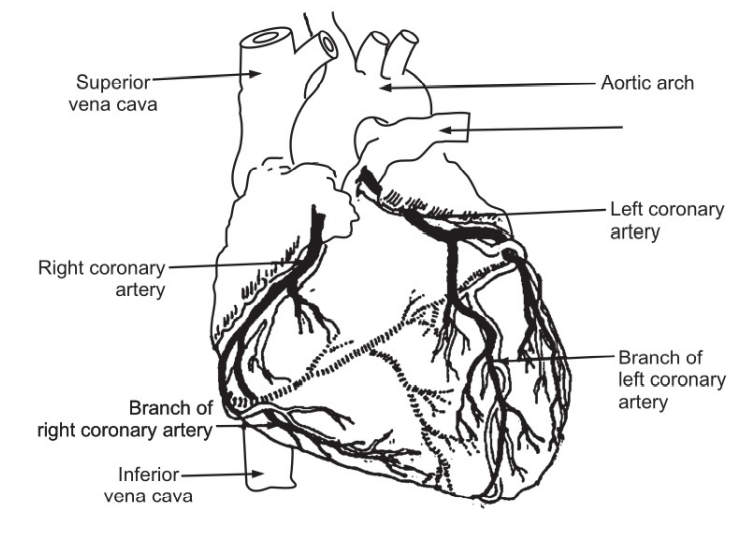
Arterial circulation
The heart is supplied with the right and left coronary arteries which branch from the aorta next to the aortic valve. The coronary arteries receive about 05 percent of the blood from the heart. The coronary arteries traverse the heart, eventually by forming a large network of capillaries.
Venous circulation
Most of the venous blood is collected into several small veins that join to form the coronary sinus which opens into the right atrium. The remainder passes directly into the heart chambers through little venous channels.
CONDUCTING SYSTEM OF THE HEART
The heart has an intrinsic system whereby the cardiac muscle is automatically stimulated to contract; however it can be stimulated or depressed by the nerve impulses initiated in the brain and by the circulating neurotransmitters or hormones. There are small groups of specialized neuromuscular cells in the myocardium which initiate and conduct impulses causing coordinated and synchronized contraction of the heart muscle.
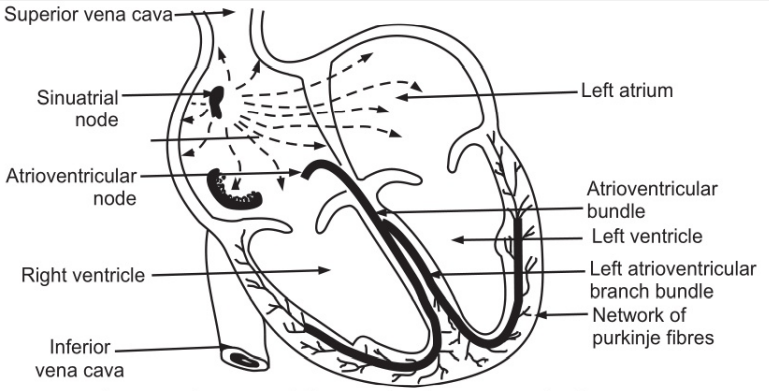
Sinoatrial Node (SA node)
It is a small mass of specialized cells in the wall of the right atrium near the opening of the superior vena cava. The SA node is termed as the ‘pace-maker’ of the heart. Normally, it initiates impulses more rapidly than other groups of the neuromuscular cells.
Atrioventricular Node (AV node)
It is a small mass of neuromuscular tissue, situated in the wall of the atrial septum near the atrioventricular valves. Normally, the AV node is stimulated by impulses initiated in the atrial myocardial; however, it is also capable of initiating impulses which can cause contractions at a rate slower than that of the SA node.
Atrioventricular bundle: (AV bundle or bundle of HIS)
It consists of a mass of specialized fibers originating from the AV node. The AV bundle crosses the fibrous range that separates the atria and ventricles. At the upper end of the ventricular septum, it divides into right and left bundle branches. Within the ventricular myocardium, the branches break into fine fibers, called the Purkinje fibers. The AV bundle, bundle branches, and Purkinje fibers convey impulses of contraction from the AV node to the apex of the myocardium where the wave of ventricular contraction begins, then sweeps upwards and outwards, pumping blood into the pulmonary artery and the aorta.
Nerve supply to the heart
In addition to the intrinsic impulses generated within the heart, it is also influenced by autonomic nerves originating in the cardiac center in the medulla oblongata which reaches through the autonomic nervous system. It is controlled by both parasympathetic and sympathetic nerves. The vagus nerves (parasympathetic) supply mainly the SA, AV node, and atrial muscle. Stimulation of the vagus reduces the heart rate and the force of contraction. The sympathetic nerves supply the SA and AV node and the myocardium of the atria and ventricles. Sympathetic stimulation increases the rate and force of contraction.
Factors affecting Heart Rate
Following are the factors influencing the heart rate:
- Autonomic nervous system.
- Circulating neurohormones.
- Exercise.
- Emotional states.
- Gender.
- Age.
- Temperature.
- Baroreceptor reflex.
The Cardiac Cycle
The heart acts as a pump and its action consists of a series of events known as the cardiac cycle. During each cardiac cycle, the heart contracts and then relaxes. The period of contraction is called systole and that of relaxation, diastole.
Normally, there are 60-80 cardiac cycles per minute. Taking 74 as the average number of cardiac cycles per minute, every cycle lasts for about 0.8 seconds. Each cycle consists of the following events:
- Atrial systole-contraction of the atria.
- Ventricular systole-contraction of the ventricles.
- Complete cardiac diastole relaxation of the atria and ventricles.
The sequence of events of a cardiac cycle is related to the flow of blood from the beginning of one heartbeat to the beginning of the next beat.
The superior vena cava and the inferior vena cava transport deoxygenated blood into the right atrium; simultaneously four pulmonary veins convey oxygenated blood into the left atrium. The atrioventricular valves are open and blood flows through to the ventricles. The SA node emits an impulse which stimulates a wave of contraction that spreads over the myocardium of both atria, emptying the atria and completing ventricular filling. This entire event lasts for 0.1 seconds and is termed as atrial systole.
When the wave of contraction reaches the AV node, it is stimulated to emit an impulse which quickly spreads to the ventricular muscle via the AV bundle, the bundle branches, and Purkinje fibers. This results in a wave of contraction which sweeps upwards from the apex of the heart and across the alls of both ventricles pumping the blood into the pulmonary artery and the aorta. This event, lasting for 0.3 seconds is termed as ventricular systole. The high pressure generated during ventricular contraction is greater than that in the aorta and forces atrioventricular valves to close.
After contraction of the ventricles, there is complete cardiac diastole, lasting for about 0.4 seconds, during which both atria and ventricles relax. During this time the myocardium recovers until it is able to contract again.
Electrical Changes in the Heart
Since the body fluids and tissues are good conductors of electricity, the electrical activity within the heart can be detected by attaching electrodes to the surface of the body. The pattern of electrical activity can be displayed on an oscilloscope screen or traced on paper. The instrument, on which it is recorded, is termed an electrocardiograph; and the tracing is termed as the electrocardiogram (ECG). The normal ECG tracing shows five waves which have been named P, Q, R, S, and T.
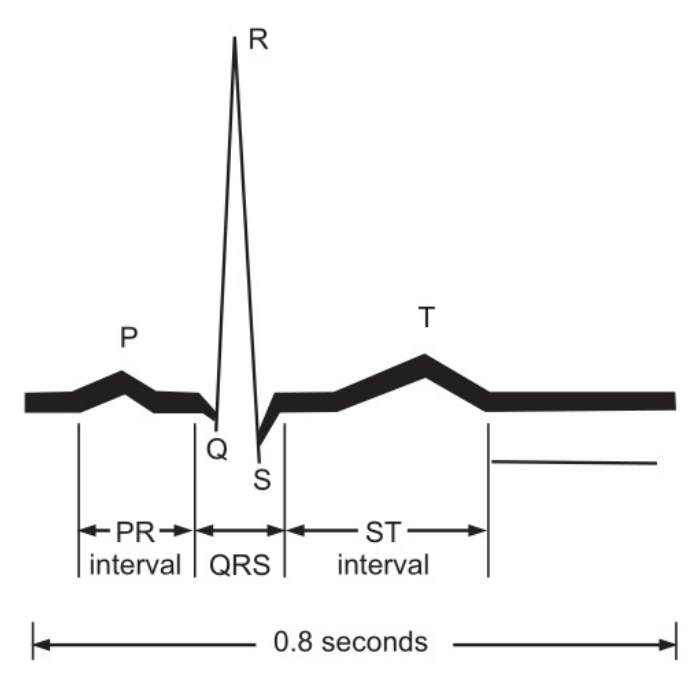
The P wave arises when the impulse from the SA node sweeps over the atria. The QRS complex represents the very rapid spread of the impulse from the AV node through the AV bundle and the Purkinje fibers and the electrical activity of the ventricular muscle. The T wave represents the relaxation of the ventricular muscle. The ECG originates from the SA node and is known as sinus rhythm. The rate of sinus rhythm is 60-100 beats per minute. A faster heart rate is called tachycardia and a slower heart rate is termed as bradycardia. By examining the pattern of ECG waves and the time interval between cycles, pathological changes within the myocardium and conducting system of the heart can be diagnosed.
Cardiac output
The cardiac output is the amount of blood ejected from the heart. The amount expelled by each contraction of the ventricles is called as stroke volume. Cardiac output is expressed in liters per minute (l/min) and is calculated by multiplying the stroke volume by the heart rate (beats /min).
Cardiac output (l/min) = Stroke volume (ml) x Heart rate (beats/ min).
In a healthy adult at rest, the stroke volume is approximately 70 ml considering the heart rate to be 72 beats/min; the cardiac output is 05 l/min. This can be greatly increased during exercise to around 25 l/min. or 35 l/min in the case of athletes. This increase during exercise is called cardiac reserve. When increased blood supply is needed for higher requirements of tissues for oxygen and nutrients, heart rate and /or stroke volume can be increased. Following factors influence heart rate.
- Autonomic nervous system.
- Gender.
- Age
- Body temperature
Stroke Volume
The stroke volume is determined by the volume of blood in the ventricles immediately before they contract, i.e. the Ventricular end-diastolic Volume (VEDV), also termed as preload. It depends on the amount of blood returning to the heart through the superior and inferior venae cavae; termed as a venous return. Increased VEDV leads to stronger myocardial contraction, and more blood is expelled. In turn, the stroke volume and cardiac output are increased. The capacity to increase the stroke volume with increasing VEDV is finite. Above this limit, the heart starts failing. Other factors which increase myocardial contraction are:
- Increased stimulation of the sympathetic nerves supplying the heart.
- Hormones, e.g. adrenaline, nor-adrenaline, thyroxin.
Arterial blood pressure affects the stroke volume because it creates resistance to the flow of blood. This resistance is termed as after-load. It is determined by the elasticity of the large arteries and the peripheral resistance of arterioles. Blood volume is normally kept constant by the kidneys. If stroke volume is deficient, it will reduce the blood flow. It will decrease the cardiac output and venous return. Venous return is the major determinant of cardiac output and, the heart pumps out all the blood returned to it. The force of contraction of the left ventricle ejecting blood into the aorta is not sufficient to return the blood through the veins and back to the heart. Following are additional factors influencing the venous return:
- Position of the body.
- Muscular contraction.
- Respiratory pump.
Make sure you also check our other amazing Article on: Anatomy Of Ear