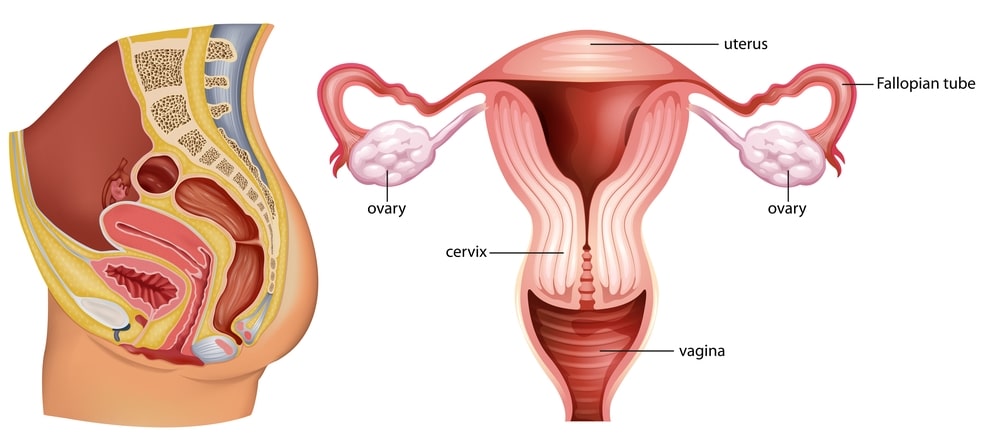
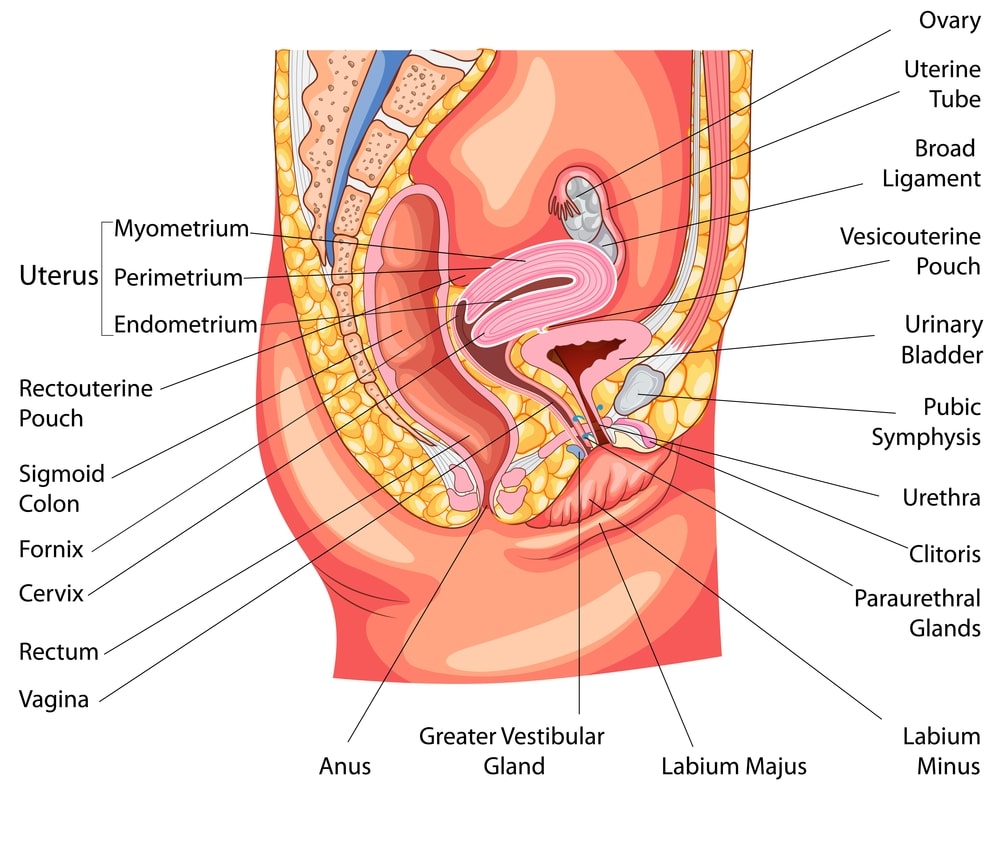
The female reproductive system consists of the following organs:
- External genital organ: Mons pubis, Labium majus [labium majus podendi], Labium minus [labium minus podendi], clitoris and the hymen.
- Internal genital organs: Vagina, uterus, ovaries and fallopian tubes.
- Accessory organs: Breast.
Table of Contents
Vagina
It is a tube-like structure that works as a passage for childbirth and menstrual flow. The semen is deposited during sexual intercourse in the vagina. It is composed of fibromuscular tissues lined with mucous membranes. It is about 04-06 ishes in length and supplied with blood vessels and nerves. It is present between the rectum and urinary bladder. Superiorly, it is attached to the uterus. The vaginal mucosa is continuous with the uterus. The mucosa is composed of non keratinized stratified squamous epithelial cells and areolar tissues. These help for transverse folds called rugae. The mucosa contains glycogen. After decomposition of glycogen, it is converted into organic acids. These acids assist in killing micro-organisms (also) have the ability to destroy the sperms in the vagina. The alkaline nature of the seminal fluid neutralizes the acidity in the vagina and helps in maintaining its viability.
The muscular part is composed of the circular that lies to the outside and a longitudinal layer on the inner side. This layer is composed of smooth muscles which can stretch sufficiently during sexual intercourse to receive the penis.
The superficial layer of the vagina called the adventitia is composed of areolar connective tissue. At the vaginal orifice, there is a thin membrane called the hymen. It forms the border of the orifice.
Vulva
The various parts of the vulva are as follows:
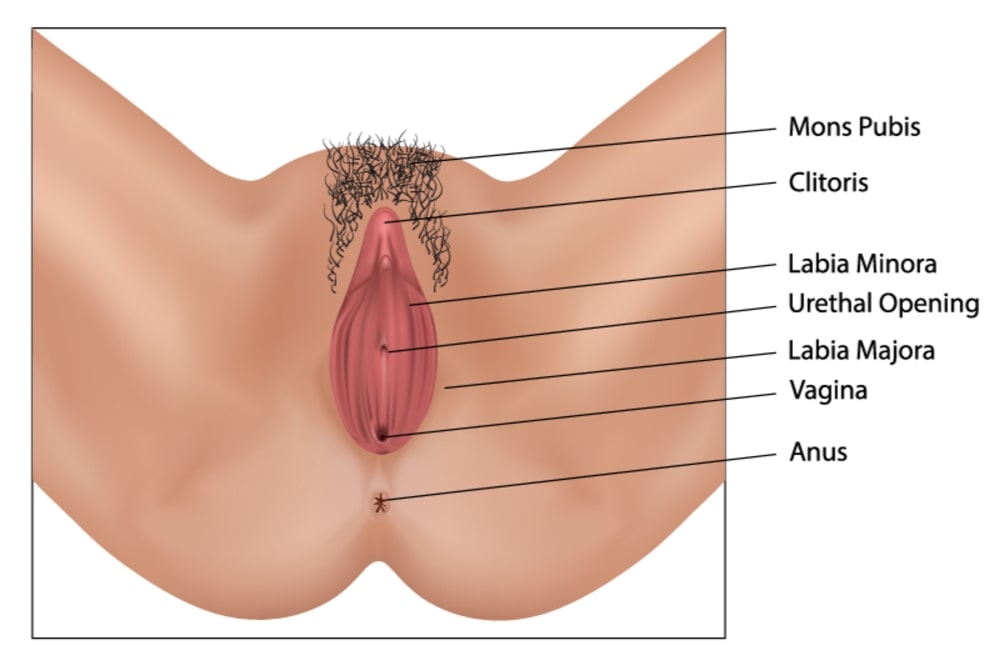
Mons pubis
It lies anteriorly to the urethral and vaginal openings. It is chiefly composed of adipose tissue and covered with skin and pubic hair.
Labia Majora
These are two longitudinal folds, extending from the Mons pubis and composed of adipose tissue, sebaceous glands, and sweat glands and are covered by hair.
Labia Minora
These are two smaller folds lying medially to the Labia Majora. These are also composed of fatty tissue, sebaceous gland, and sweat glands.
Clitoris
It is a small, cylindrical mass of erectile tissue, lined with nerves. It lies anterior to the Labia Minora. The foreskin is present at the junction of the Labia Minora which covers the clitoris. The clitoris is erotogenic.
Vestibule
The space present between the two Labia Minora is known as the vestibule. This space is occupied by the vaginal orifice, the hymen and the external urethral orifice. Deep within the labia, on both sides of the vaginal orifice erectile tissues are present. This tissue helps to narrow the vaginal orifice during sexual intercourse which puts pressure on the penis. The external urethral orifice helps in expelling urine. Paraurethral glands are seen on the inside wall of the urethra. They secrete mucously. Bartholdi’s glands are present at the vaginal orifice. They secrete mucous during sexual contact which provides lubrication.
Mammary Glands
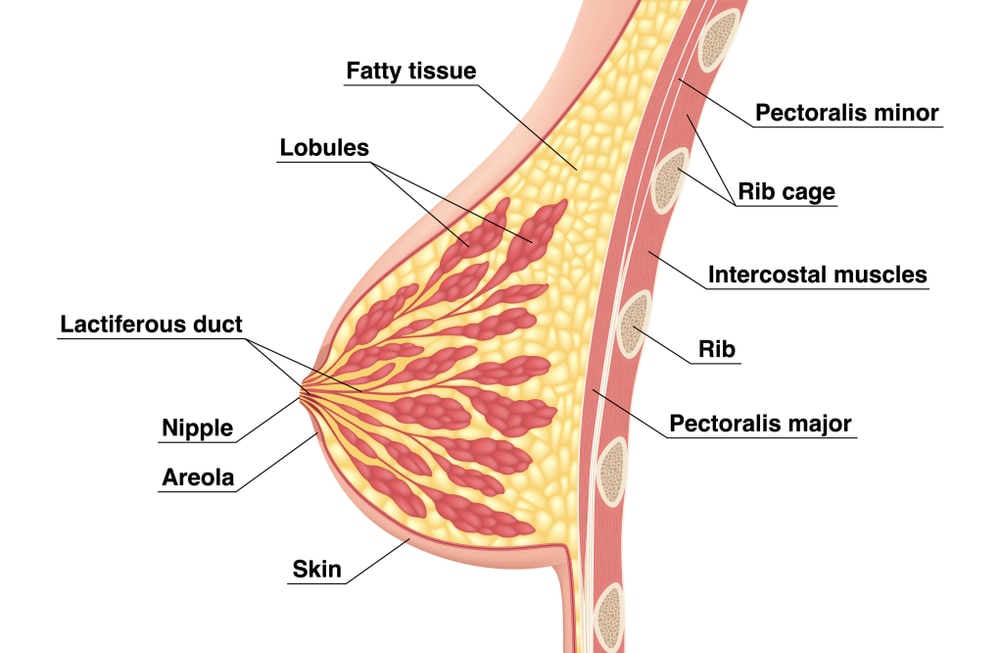
These are modified sweat glands, responsible for the production of milk. The breast shows the presence of the nipple. Behind the nipple several small ducts known as lactiferous ducts are present. Modified sebaceous glands are present around the nipple. This space is known as the areola. The breast is supported by suspensory ligaments, which pass through the skin lying deep inside the breast tissues. Each breast consists of 16-22 lobes. The lobes are separated by adipose tissue. The lobes consist of small spaces known as lobules. These lobules show the presence of secreting glands called alveoli which are supported by connective tissues. The alveoli are surrounded by myoepithelial cells. Due to the contraction of myoepithelial cells milk is pushed towards the nipple. Due to the expansion of ducts, sinuses are formed where the milk is stored. The lactogenic hormone assists in milk secretion. This function is associated with childbirth. The hormone oxytocin assists in the contraction of the myoepithelial cells, pushing the milk towards the nipple in the process.
Ovary
These are female gonads, lying in a shallow cavity on the lateral wall of the pelvis, one on each side of the uterus. These are attached to the uterus by a broad ligament called mesovarium. The size of the ovary is variable. The length is 02.5-03.5 cm, the breadth is 02 cm and thickness is 01.25 cm.
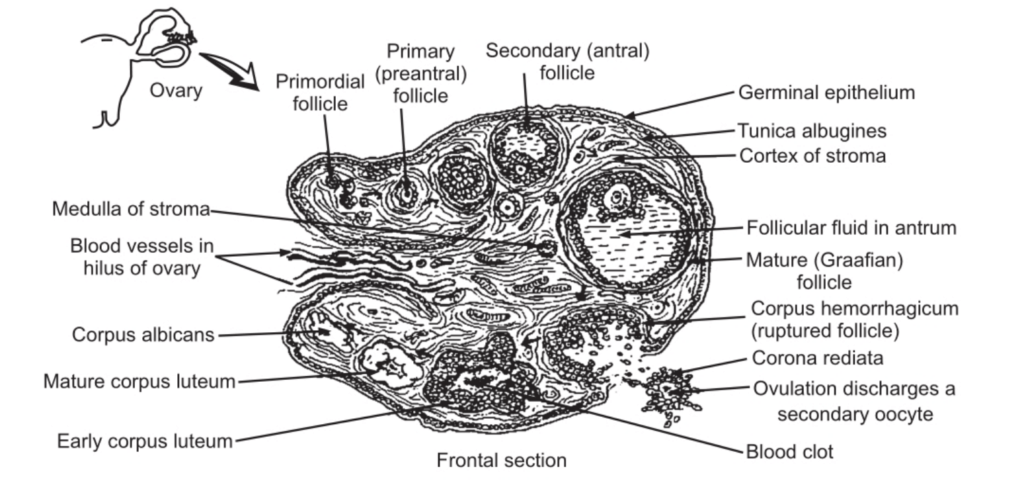
The ovaries are divided into the cortical part and medullary part.
The medulla consists of fibrous tissues in which blood vessels, lymphatic vessels and nerves are present.
The ovary shows different parts:
The Germinal Epithelium
The surface of the ovary is covered by simple epithelial tissue. This layer is called the germinal epithelium. Below the germinal epithelium, dense irregular connective tissue called tunica albuginea is seen. Another layer of connective tissue, lying below the tunica albuginea known as stroma is observed. The dense layer of the stroma is called the cortex and the loose layer of the connective is known as the medulla. The cortex shows the presence of ovarian follicles which contain oocytes in various stages of development. The surrounding cells provide nourishment to the oocytes and also secrete the hormone oestrogen. A fully matured Graafian follicle ruptures and releases the ovum. This stage is known as ovulation. The empty ruptured ovarian follicle is known as the corpus enteum. This produces the hormone, progesterone until it degenerates and is converted into the fibrous tissue known as corpus Albicans.
Fallopian (Uterine) Tubes
These are two tubes, lying one on each lateral side of the uterus. They are approximately 10 cm in length, upper free border ligaments of the uterus. These oviducts are responsible for the transport of oocytes as well as fertilized ova from the ovaries to the uterus. The funnel-shaped part of the fallopian tube at the opening end is known as the infundibulum. The infundibulum has finger-like projections known as fimbriae. The uterine tube has three layers: the outer serosal, which is a serous membrane, the middle layer, a muscular layer containing circular and longitudinal layers of smooth muscles and the inner layer which is mucosa, containing ciliated columnar epithelial cells which help in the movement of the fertilized ovum. Due to the peristaltic action of the muscular, the ovum is propelled along the tubes.
Uterus
It is present between the bladder and the rectum. The uterus is the site for implantation of the fertilized ovum, development of the embryo and foetus and also for menstruation. The uterus is an inverted pear-shaped organ. It is 07.5 cm long, 05 cm wide and the thickness of its wall is about 02.5 cm. The uterus is divided into three parts, i.e. the fundus, body and cervix. The expanded superior part, lying above the opening of the fallopian tube is known as the fundus.
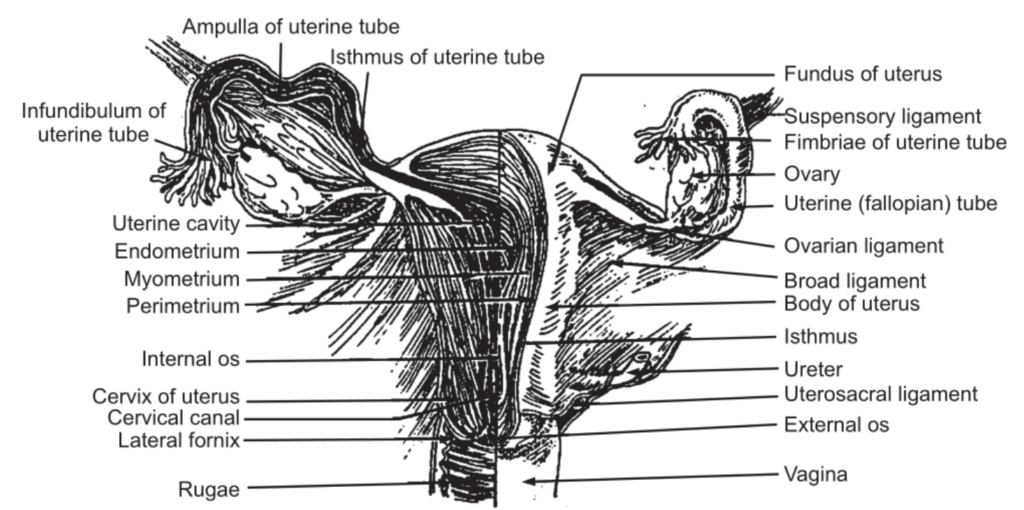
The narrow and constricted part towards the inferior side is the body. The narrow part in the neck region that emerged into the anterior wall of the vagina is called the cervix. The space within the uterus is known as the uterine cavity. The position and range of movement of the uterus are controlled by three pairs of suspensory ligaments. The wall of the uterus consists of three main layers, the inner endometrium, the middle layer, the muscular myometrium, and the outer layer, the serosal or perimetrium. The endometrium is a mucous membrane and contains three layers. The stratum compactum is the outer compact surface layer of ciliated, columnar epithelium. The spongy middle layer is the stratum spongiosum which consists of loose connective tissue. The dense inner layer is the stratum basal which underlies the myometrium. The functional part of the endometrium nourishes the developing embryo. But after childbirth or during menstruation nourishment is slowed down as the levels of the hormone, oestrogen and progestogen are reduced. The bulk of the uterine wall is formed by the myometrium which is thick in the fundic region and thin in the lower cervical part. This structure helps in expelling the foetus. The fundic region contracts more forcibly than the cervical region, and it helps to dilate the cervix and encourage childbirth.
Menstrual Cycle
At the age of 12-14 years, the menstrual cycle starts. This is the age of puberty. The onset of menstruation is known as menarche. The reproductive organs, the uterus, the vagina and the breasts start enlarging with an increase in fat deposition, the number of blood vessels and connective tissues. There is an appearance of secondary sex characteristics.
Menopause
At the age of 40-45 years, the reproductive system ceases to function. The menstruation cycle stops and the ovary and breasts begin to diminish in size.
Hormonal Regulation
Hormones regulate the menstrual cycle. The hormone gonadotropins released from the hypothalamus controls the secretion of the follicle-stimulating hormone (FSH) and the luteinizing hormone (LH) from the anterior pituitary gland. The FSH is responsible for the development of ovarian follicles and stimulates ovarian cells to secrete oestrogen. The LH stimulates further development of ruptured follicles and stimulates these cells to secrete progesterone Relaxin and Inhibin.
Oestrogen
This hormone has some important functions. It influences the development and maintenance of the female reproductive system, and the development of secondary sex characteristics, like distribution of adipose tissue in the breasts, hips, mons pubis, and abdomen, hair growth on the head and body, voice pitch, and broadening of the pelvis. The hormone controls the electrolyte balance, assists in protein anabolism and in lowering the blood cholesterol level. Progesterone secreted from the corpus luteum, along with oestrogen prepares the endometrium for implantation of the fertilized ovum and the mammary glands for milk secretion.
The hormone relaxin helps in relaxing smooth muscles of the uterus. The hormone also relaxes the pubic symphysis. This enlarges the cervix helping in the easy delivery of the baby. The Inhibin hormone secreted by growing follicle cells called granulosa cells and by the corpus luteum inhibits the secretion of FSH and to some extent of LH.
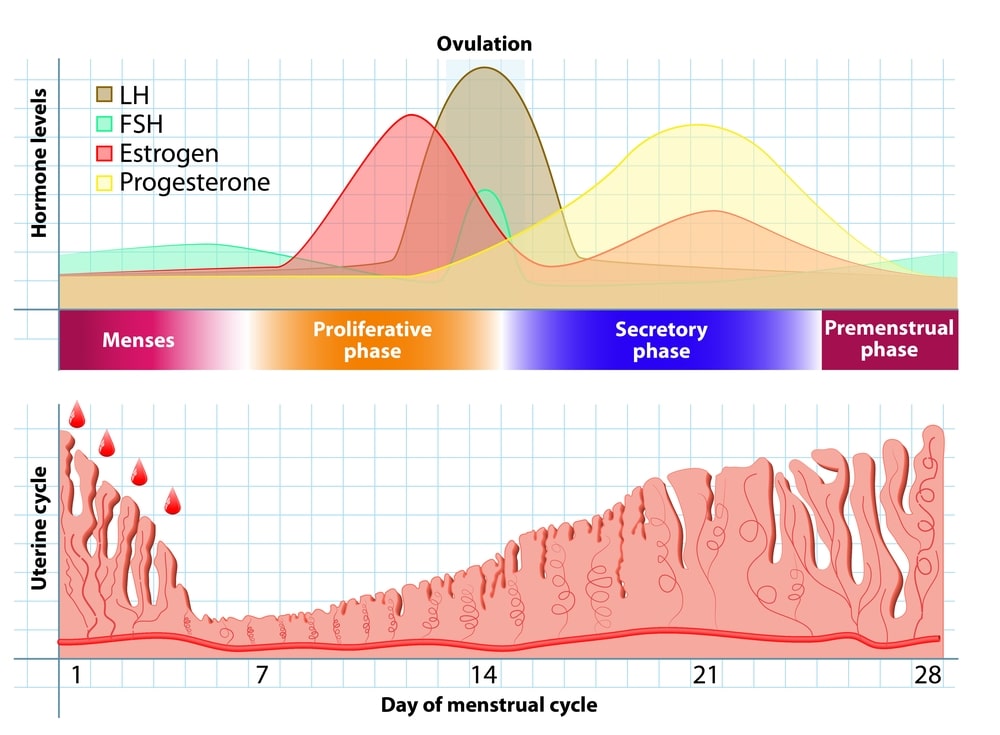
The menstrual cycle takes place in a series of events that occur at regular intervals over a period of about 28 days. There are mainly three phases.
- The proliferative phase.
- The secretory phase.
- The menstrual phase.
The Proliferative phase
Various events take place during this phase. The gonadotropic hormone, FSH secreted from the pituitary gland, passes into the bloodstream and reaches the ovary. The hormone exerts a local effect upon the ovary. It stimulates the growth and development of the ovarian follicle. The ovarian follicle contains the ovum, which starts to grow and develop. Normally, one ovum grows and develops, but sometimes more than one ovum also grows, develop and matures. After the full maturation of the ovum, the ovarian follicle ruptures and the matured ovum leave the ruptured follicle and enter the peritoneal cavity. This process of release of the ovum from the ruptured follicle is known as ovulation. The released ovum is captured by the fimbriated end of the fallopian tube and pushed along the fallopian tube towards the uterus. This is carried out by peristaltic action.
Under the effect of FSH, the ovarian follicle grows and matures. At the same time, under the influence of FSH, the cells of the ovarian follicle secrete the hormone oestrogen. Oestrogen enters the blood to reach the endometrium where it stimulates the cells of the endometrium. As a result, the columnar cells of the endometrium reproduce more rapidly to form a thicker lining of the walls of the endometrium. The number of glands and blood capillaries also increases.
The Secretory Phase
As soon as ovulation occurs, the walls of the ovarian follicle collapse. In this phase, FSH is withdrawn by the pituitary gland as the levels of oestrogen are high in the blood. Instead, it starts to secrete the second gonadotropic hormone, the luteinizing hormone. The LH enters the bloodstream reaches the ruptured follicle and influences the ruptured follicle to grow rapidly. The ruptured follicle gets filled with a yellow substance called lutein. This body is known as the corpus luteum. The cells of the corpus luteum under the influence of LH start secreting the second ovarian hormone, progesterone which is directly absorbed into the bloodstream. It exerts an effect on the endometrium, assisting the action of oestrogen. This causes an increase in the linings of columnar cells and an increase in the number of secretory glands and blood capillaries. Due to an increase in the number of blood capillaries, they form a network. The glands present in the uterine walls secrete a sticky fluid substance. Hence, this phase is known as the secretory phase.
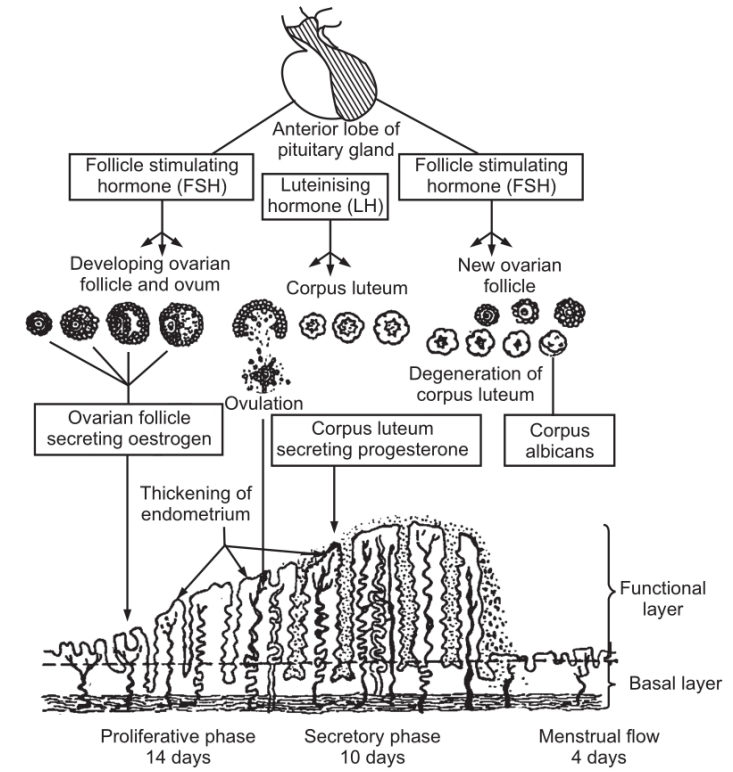
During this phase, the endometrium becomes thick, soft, moist and rich in blood capillaries. The endometrium undergoes these structural changes so that the fertilized ovum can be received.
The Menstrual phase
If the ovum is not fertilized the activity of the pituitary gland is reduced due to high levels of progesterone which inhibits the activity of the pituitary gland also causing a reduction in the level of the luteinizing hormone. Due to the withdrawal of the luteinizing hormone, degeneration of the corpus luteum takes place. This in turn helps the level of progesterone. Once the reduced progesterone levels fall, the endometrium inside the uterus breaks down, the cells lining the uterus disintegrate and blood capillaries break down. The extra secretion, lining endometrium cells blood from the broken capillaries and the unfertilized ovum constitute the menstrual flow.
Once the progesterone level in the blood decreases to a certain level, the pituitary gland begins to secrete the FSH. Another ovarian follicle is stimulated and the cycle goes on again.
In the event when the ovum is fertilized, the endometrium does not break down and there is no menstrual flow. The fertilized ovum embeds itself within the endometrium and the chorionic gonadotropins are produced. This hormone keeps the corpus luteum in an intact condition so that it keeps secreting the progesterone continuously. The fertilized ovum during the first twelve weeks is called the embryo and thereafter it is known as a foetus. This foetus is protected and nourished for nine months within the uterus. After the full term is reached, the baby is ready to be born.
Make sure you also check our other amazing Article on: Male Reproductive System