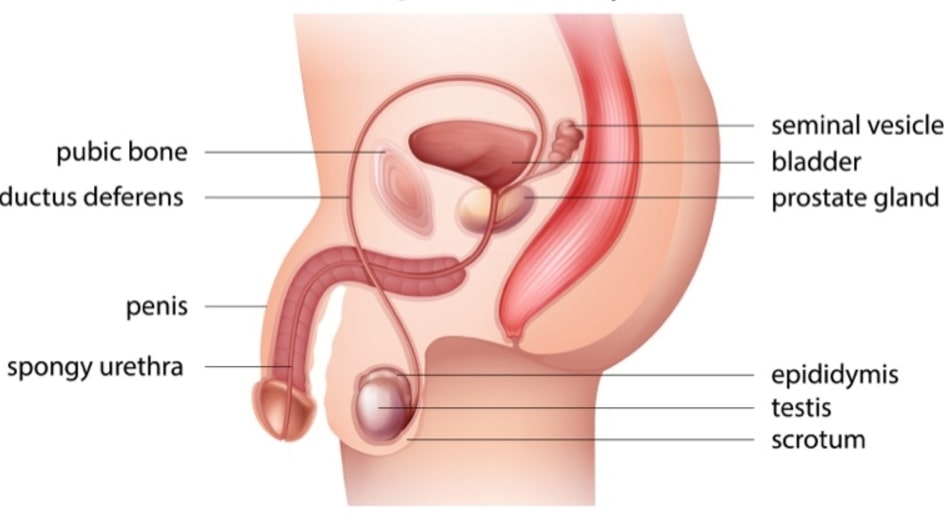
The Male Reproductive System are classified into external genital organs, i.e. scrotum, penis and urethra and internal genital organs, namely, testes, vas deferens, seminal vesicle and prostate gland.
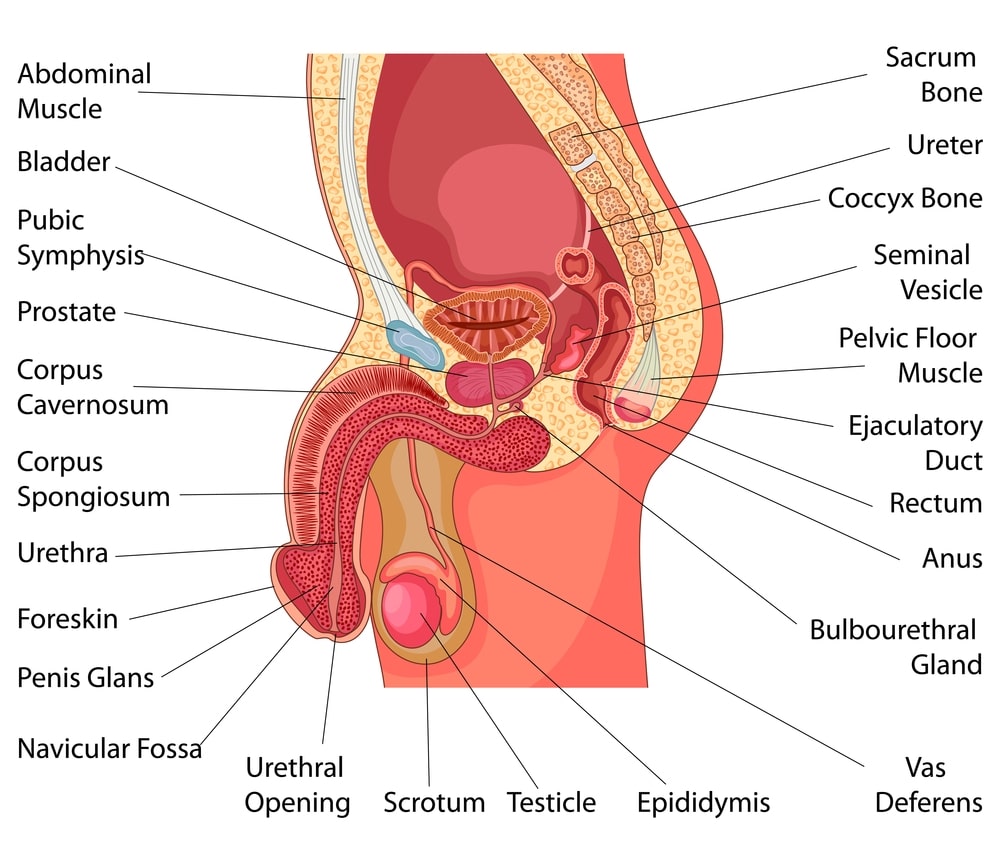
Table of Contents
Scrotum
It is a sac-like structure and hangs from the root of the penis. It consists of loose skin and superficial fascia, that support testis. There are two sacs, which divide vertically, each one containing testis. The muscle composed of smooth muscle fibres acts as a septum. A temperature of 03°C is essential for the survival of sperms which is obtained due to the contraction of muscle fibres. In the spermatic cord, a small band of skeletal muscles is present, which is known as the cremaster muscle.
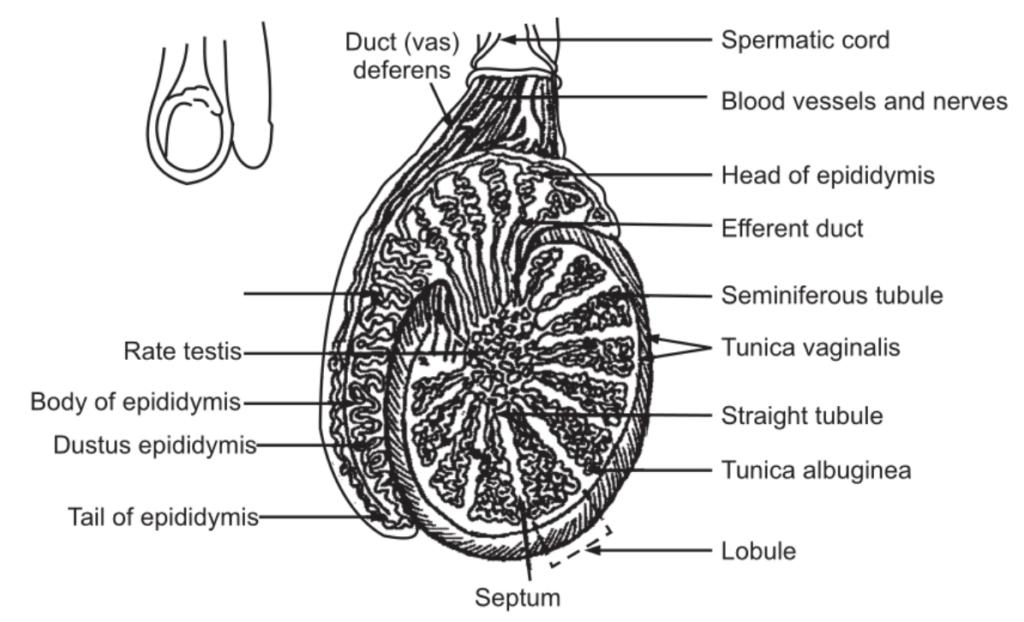
The Testes
These are two in number. Each one is about 05 cm long and 2 1/2 cm in diameter. The weight of each is 10-15 gm. The testes are covered by a serous membrane called tunica vaginalis. Inside the tunica vaginalis, is the tunica albuginea, composed of the dense white fibrous capsule. The tunica albuginea (goes inwards) forms a septum so that the testis is divided into several internal compartments known as lobules.
Tightly coiled tubules called somniferous tubules are present in the lobules. They serve as the site for the production of sperms.
The sperm forming cells are called spermatogenic cells. These cells line the somniferous tubules along with supporting cells. They undergo mitosis to eventually produce sperm. The immature spermatogenic cells are known as spermatogonia. These lie next to the basement membrane. Towards the lumen of the tubule more mature cells are present. These are primary spermatocytes, secondary spermatocytes, spermatids and sperms. As the spermatozoon reaches maturity, spermatozoon is released into the lumen of the somniferous tubule. Between the spermatogenic cells, sustentacular cells, are present which extend from the basement membrane up to the lumen of the tubule. Inside the basement membrane, tight junctions join the neighbouring sustentacular cells to one another and these junctions form the blood testes barrier. For the development of gametes, various substances are essential, which must pass through the sustentacular cells. The spermatogenic cells contain surface antigens. By isolating the spermatogenic cells from the blood, the blood-testes barrier prevents an immune response against the surface antigens. The space between the somniferous tubules is occupied by interstitial cells that secrete the hormone testosterone.
Spermatogenesis
This is the process by which the somniferous tubules of the testes produce sperms. The parent cells (spermatogonia) produce sperms. This process involves fewer than four main stages in which spermatogonia, spermatocytes, and spermatids and finally spermatozoa are produced.
The spermatogonia are situated peripherally in the somniferous tubule and are large cells. They undergo meiotic division to give rise to spermatocytes.
Spermatocytes can be differentiated into two types: primary spermatocytes and secondary spermatocytes. The primary spermatocytes in humans contain 46 chromosomes. Out of these 44 are autosomes and two are sex chromosomes. In autosomes, all cells have a similar shape. The primary spermatocytes by meiosis give rise to secondary spermatocytes which contain 23 chromosomes of which 22 are autosomes and one is a sex chromosome. In the testes, male gametes are produced. These are known as sperms. Ovaries in females produce female gametes known as ova. By the union of male and female gametes, a zygote is produced; which contains chromosomes (DNA) of mother and father the total chromosomes in the offspring are 46 in number: 23 chromosomes from the mother and 23 chromosomes from the father.
In the seminiferous tubules, spermatozoa are situated centrally whereas spermatogonia are situated peripherally. The spermatocytes and spermatids take up an intermediate position. The entire process of spermatogenesis takes approximately 72-74 days. As the individual reaches puberty spermatogenesis starts and continues up to old age; hence men remain fertile even in old age. However, females after menopause become unfertile.
Activity of Testes
The activity of the testes is controlled by hormones.
The follicle-stimulating hormone (FSH) controls spermatogenesis and secretion of testosterone are controlled by the luteinizing hormone (LH). Testosterone is derived from cholesterol in the testes and is a lipid-soluble hormone. The hormone which is produced in the interstitial cells diffuses out to enter the interstitial fluid and finally the bloodstream. The prostate gland and seminal vesicles contain a 5-alpha-reductase enzyme that converts testosterone into dihydroxy-testosterone which is more potent than testosterone. Both these hormones are used for the development of the reproductive system.
Adrenal Cortex
It is believed to control the differentiation of sex in the foetus, the growth of sex glands, sex organs and secondary sex characteristics after birth. The adrenal cortex secretes sex hormones.
Thyroid
The thyroid glands and gonads stimulate each other. This relation is mediated through the anterior pituitary.
Morphological Structure of Spermatozoon
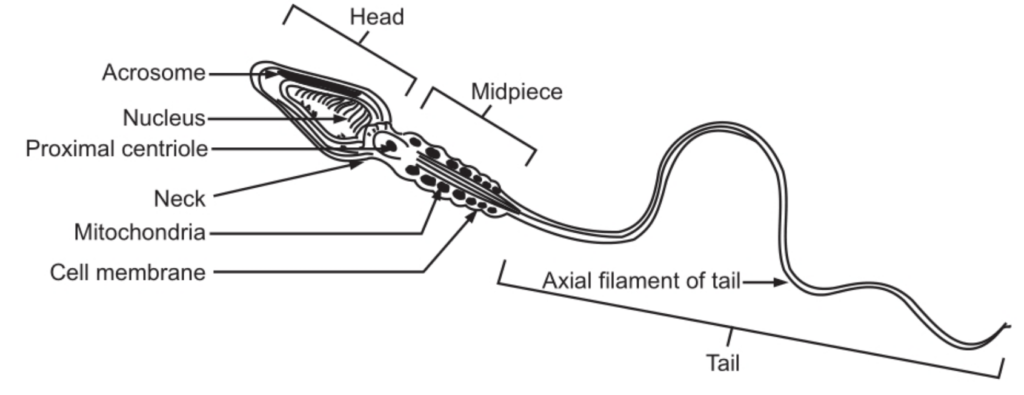
A fully matured spermatozoon is about 62 μm long which is divided into head and tail which is a single cell. DNA is present in the nucleus, which forms the head. This head is covered by acrosome which is made up of mucopolysaccharide and acid phosphates. The tail is divided into several parts, i.e. neck, middle piece, principal piece and end piece. This shape of the spermatozoon facilitates its entry into the female genital tract. The body of the spermatozoon contains phospholipids. The spermatozoon can survive for long periods. The Semen
About 02-05 ml of semen comes out during each ejaculation and clots after ejaculation. After about 15 minutes this clot liquefies. During intercourse, the semen is deposited deep in the vagina. In normal human beings, the seminal fluid contains sperms and seminal plasma. In a healthy person, the sperm count varies from 40 x 105 – 100 x 10°. About 65 per cent of the sperms remain motile after an hour in a hanging drop preparation.
The semen is alkaline in reaction. It is composed of ascorbic acid, citrate, acid phosphates and fructose. Fructose is the main fuel for the spermatozoon; the pH of semen is 07.2-07.7. For artificial insemination, the semen is stored under-78°C. 2.
Penis
This is the male genital organ for reproduction. The penis also contains the urethra. The urethra is used for the ejaculation of semen and excretion of urine. It has a cylindrical shape and consists of the glans penis, the root and the body. The body of the penis contains three cylindrical masses of tissue which are bound by fibrous tissues known as tunica albuginea.
The dorsolateral masses are called the corpora cavernous penis. Inside the corpora, cavernous is the midventral mass called the corpus spongiosum penis. This layer helps to form a spongy urethra and is kept open for ejaculation. This layer of the urethra consists of erectile tissue which contains blood sinuses. All the layers are covered by fascia and skin. Sexual stimulation may occur by visual, tactile, auditory, olfactory stimuli or even by imagination, whereupon the blood vessels that supply blood to the penis dilate. The dilation of blood vessels causes maximum blood to enter into the blood sinuses; there is an expansion of spaces, and the veins get compressed. The blood that enters into sinuses is trapped. These vascular changes lead to an erection. The penis comes to its original shape when the arteries are constricted and pressure on the veins is relieved. Sympathetic reflex action helps for ejaculation and the sphincter muscle at the base of the urinary bladder closes, because of which urine is not expelled out during ejaculation, and the semen does not enter the urinary bladder.
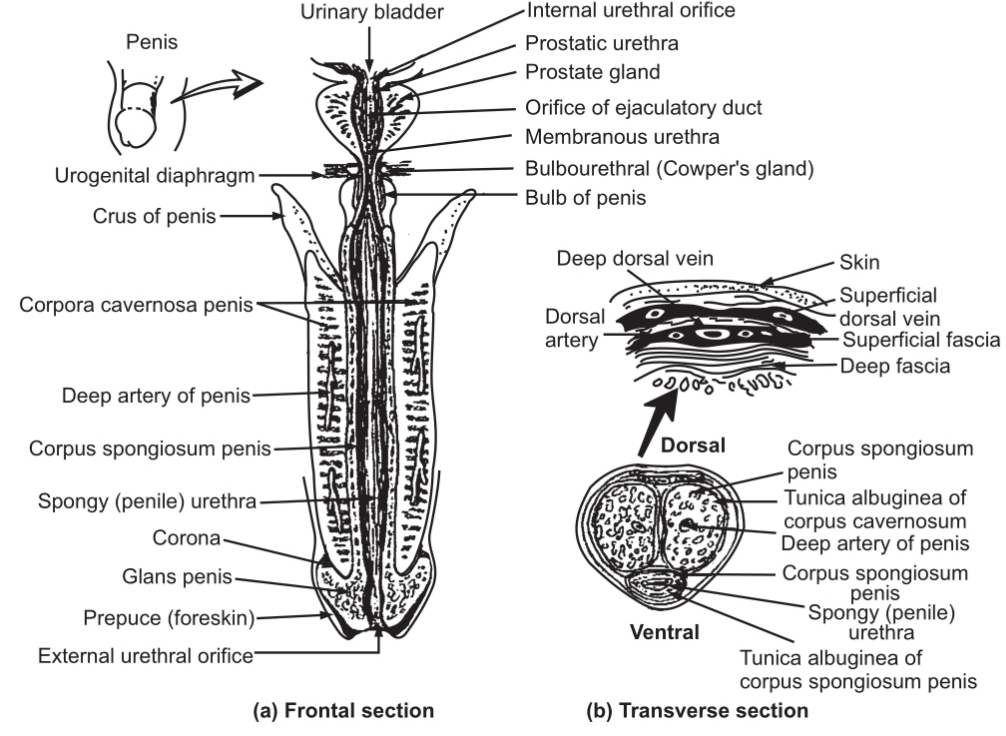
The root of the penis is a proximal portion, containing the bulb of the penis. The bulb is attached to the inferior surface of the urogenital diaphragm. The bulb of the penis is the expanded part of the base of the corpus spongiosum (penis) and the curare of the penis. Due to the contraction of these muscles, ejaculation occurs.
The distal end of the corpus spongiosum (penis) is enlarged and is called as glens penis. The marginal part of the glans penis is known as the corona. The urethra at the end forms the enlarged external urethral orifice. The glens are covered by the foreskin.
The Epididymis
It is a long comma-shaped organ that is about 04 cm in length. It lies on the posterior border of the testes and is coiled in appearance. The larger part of the duct is known as the head. The body lies in the middle part and the tail lies to the inferior side. The tail continues as vas deferens. The epididymis is a tightly coiled structure and is about 06 metres in length. Its walls are composed of pseudostratified columnar epithelium and smooth muscles. At the surface of the columnar cells branching microvillus, called stereocilia are present. This structural feature enhances the surface area which proves helpful in the reabsorption of degenerated sperms.
Vas Deferens
The tail of the epididymis is known as vas deferens. It is about 45 cm in length. Its dilated part is called the ampulla. Its walls are composed of three layers of cells. The inner and outer layers are composed of longitudinal muscle fibres and the middle layer is composed of the circular muscle layer. Vas deferens normally stores the sperms. These sperms remain viable for several months. The ejaculatory duct which is about 02 cm long helps in ejaculation. The semen is forcefully expelled from the urethra to the outside.
Urethra
It forms the terminal part of the duct of the urinary and reproductive system. Its function is to throw the semen and urine outside. It is 20-22 cm long and passes through the prostate gland, the urogenital diaphragm and the penis. The prostatic urethra which passes through the prostate gland is 02-03 cm. long. The spongy urethra at the end forms an external urethral orifice.
The Seminal Vesicles
These are two in number and are sac-like structures about 04-05 cm in length. The seminal vesicles are present at the (posterior and up to base) of the urinary bladder. The seminal vesicles secrete a viscous alkaline fluid that contains the sugar fructose. The alkaline nature of this fluid assists in neutralizing the acid in the female genital tract as it can be fatal for sperms. Fructose helps in ATP production by the spermatozoon. The viability, motility of sperms and muscular contraction is controlled by prostaglandins. After ejaculation, the semen clots due to a protein called semenogelin. About 60-65 per cent of the semen is secreted by the seminal vesicles.
Prostate Gland
It is a small gland present inferiorly to the urinary bladder. The prostate gland secretes milky and less acidic fluid of pH 06.4-06.5. The fluid briefly contains ionized citric acid and is used for ATP production. Apart from this, it also contains acid phosphates, prostate-specific antigen (proteolytic enzyme), pepsinogen, amylase; lipase, and hyaluronidase. The liquefaction of semen is facilitated by the prostate-specific antigen. The prostate gland surrounds the urethra. Any infection to the urethra poses a risk to the prostate gland. The size of the prostate gland is subject to change. It may enlarge and obstruct the function. The secretion of the prostate gland passes into the urethra to make the proper volume of the semen. It helps the sperms to remain motile and viable. The size of the prostate gland increases up to the age of about 30 years and remains constant up to the age of 45 years. Any infection leads to an increase in size.
Make sure you also check our other amazing Article on: Pancreas