Parenterals preparations are sterile, pyrogen-free liquids (solutions, emulsions, or suspensions) or solid dosage forms packaged in either single-dose or multidose containers.
- These preparations are administered through the skin or mucus membranes into internal body compartments.
- These include any method of administration that does not involve passage through the digestive tract.
The term parenteral is derived from the Greek word Para – outside and Enter one – Intestine. It denotes the route other than oral.
Table of Contents
History
In 1492, Pope Innocent had received a transfusion from young boys. In 1656, Christopher Wren used a sharpened hollow quill of a feather to inject crude extract of opium into the vein of a dog. J. D. Major and Johannes Elsholtz were the first who successfully injected humans in 1662 using solutions of opium. In the 1850s Alexander Wood was credited with giving subcutaneous injections using a true hypodermic syringe. Today, parenteral dosage forms are available with high standards.
Parenteral Advantages
- If the drug is not absorbed orally it can be given parenterally.
- A drug that is unstable in GIT can be given parenterally.
- Drugs that are undergoing extensive first-pass metabolism are given parentally which avoids the first-pass metabolism.
- When patients need rapid drug action in emergency situations as the onset of action of parenteral is rapid.
- The patient is uncooperative/unconscious (accident, surgery, etc.).
- Complete drug bioavailability (up to 100%) is possible.
- Prolonged drug action is possible.
- Parenteral therapy provides the means of correcting serious disturbances of fluid and electronic balances.
- When food cannot be taken by mouth, the total nutritional requirement can be supplied by the parenteral route.
- Patient compliance problems are largely avoided.
Parenteral Disadvantages
- Most inconvenient route of administration /pain upon injection.
- Generally, need a medical expert for administration (like physician or nurse usually in hospital or clinic).
- If administered by patients themselves, need good training.
- It requires strict adherence to aseptic procedures.
- It requires more time than those administered by other routes.
- Chances of improper dosing are more.
- Chances of adverse effects are more.
- The danger of blood clot formation is there.
- The drug cannot be recovered in adverse conditions as it is irreversible.
- The manufacturing and packaging requirements of parenteral dosage forms are more costly than other dosage forms.
Types of Parenterals
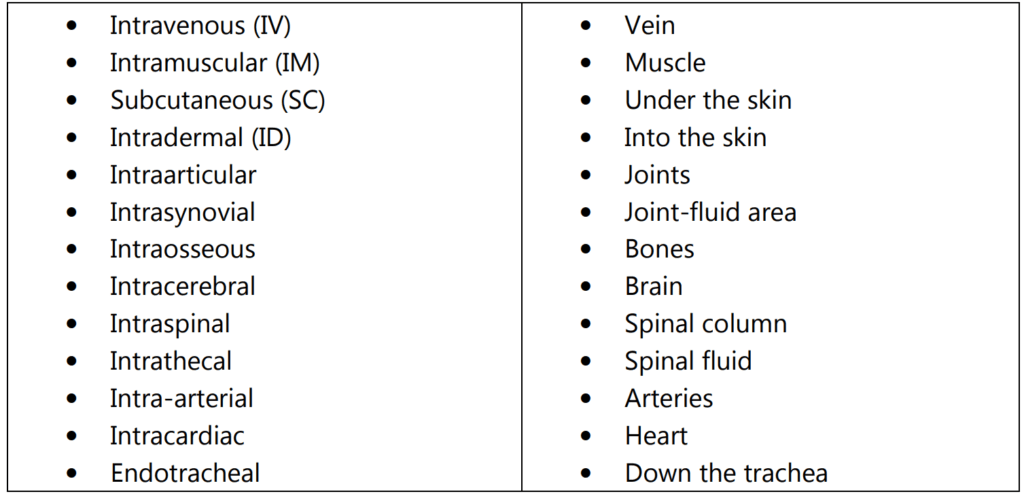
1. Based on the route of administration, the types of parenteral are:
2. Based on volume, parenteral are of Two Types:
Small volume parenteral (SVP): These are sterile, pyrogen-free injected products that are usually packed in volumes up to 100 ml.
These are aqueous preparations, usually administered by IV because of local irritation.
These SVP’s are packed into Ampoules or Vials.
Large volume parenteral (LVP): These are sterile, pyrogen-free injected products that are usually packed in volumes more than 100 mL(ranging from 101 ml to 1000 ml).
3. Based on the composition:
These products can be administered by Intra or Extravascular routes.
These LVP’s are packed into either glass or plastic containers of 1 lit capacity.

Basic Criteria for a Parenteral Preparation
- It should be sterile (free from living and detectable microorganisms).
- It should be free from pyrogens which cause the body temperature to rise.
- It should be free from visible particulate matter (which may cause embolism means blocking the blood capillaries).
- It should be isotonic (which protects the RBC).
Parenteral Products: Routes of Administration
1. Intramuscular (IM) Route
- Administration: deep skeletal muscle far from nerves & blood vessels.
- Adults: administered into the upper outer quadrant of the gluteus maximus.
- Infants: lower portion of deltoid muscle of the upper arm or mid-lateral muscle of the thigh.
- Site of injection: May vary with multiple injections.
- Note: during administration plunger of the syringe is withdrawn back to assure the absence of blood.
- 0.5 – 5 ml syringe \ 20-25 gauge \ 5/8-3″ length needle.
- Volume: maximum 5 ml in gluteus region and 2 ml in deltoid.
- Vehicle: aqueous, oleaginous, or suspension – influence duration of action.
- Advantage: suspensions can be administered.
- Less rapid than IV but has a longer duration of action.
Intramuscular (IM) Injections
- Intramuscular injections are given at 90 degrees to the skin, penetrate deep, aspirate to check whether you have punctured an artery, vein, or nerve, if blood comes, withdraw the needle, change position.
- Less rapid than IV but has a longer duration of action.
- In general, the injection of drugs into the muscle or the adipose tissue beneath the skin allows a deposit or ‘depot’ of the drug to become established that will be released gradually into the systemic circulation over a period of time.
- By changing the formulation of the drug, the period over which it is released can be influenced. For example, the formulation of antipsychotic agents such as flupentixol in oil allows them to be administered once a month or every three months.
- The danger of IM injections: It may cause paralysis, abscess, cysts, embolism, hematoma, scar formation, etc.
2. Subcutaneous (SC) Route:
- Injections in fatty subcutaneous tissues below the skin.
- Small volume injections up to a maximum of 2 ml.
- 1-3 ml syringe \ 25-32 gauge \ 1/2-5/8″ length needle.
- Site of Administration: Abdomen, upper-outer arms, upper-outer thighs, and upper back.
- At least 1 inch (2.5 cm) pinched a fold of skin and tissue is necessary for administering SC injections.
Subcutaneous Injections:
- These are given by holding the needle at a 45-degree angle while piercing the skin, skin is pinched tight.
- Put in the needle so that hub of the needle shaft touches the skin, aspirate to check the location of the needle. If blood is aspirated, withdraw the needle and try at other sites, if not gently push the medication into the subcutaneous tissue, withdraw the needle and gently massage the area to help in absorption.
3. Intradermal (ID) Route:
- The drug is administered into the dermal layer of the skin.
- Generally interior surface of the forearm.
- 1mL syringe \ 25-29 gauge \ 1/4-5/8“ (up to 1 inch).
- The usual dose is about 0.1ml.
- The needle injected horizontally into the skin with the bevel facing upward. The injection is made when the bevel just disappears.
- 5-15 degree angle with bevel up, no aspiration or massage.
Intradermal Injections:
- Intradermal injections are given by pulling the skin tight, inserting the needle, bevel up, holding it at an angle of 10 degrees as it penetrates the skin, turning the needle bevel down, and injecting a small amount of medication into the skin at the junction of epidermis and dermis until a wheel appears.
- Uses: for diagnostic determination, desensitization, or immunization.
Physicochemical Properties of the Drug
Unstable in moisture
- Dry
- Suspension
- Replace water with other solvents
Insoluble in water
- Non-aqueous solvent
- Derivative (salt)
Route of drug administration
- IV Aqueous
- Others may not be aqueous
The desired onset of drug action
- The physical state of the drug (suspension)
- Vehicle (aqueous or not)
Duration Oleaginous > suspension > aqueous
Make sure you also check our other amazing Article on : Distribution Law
