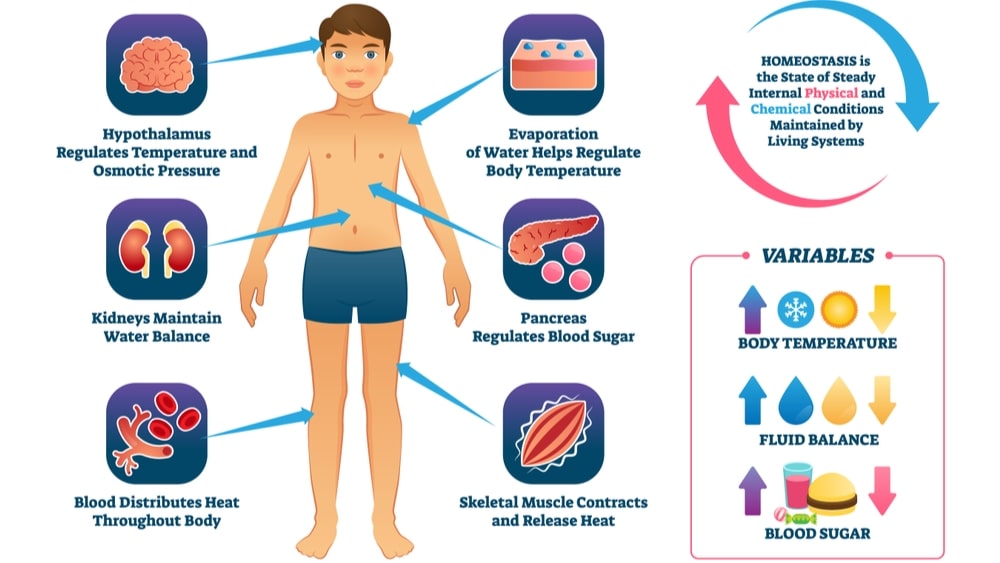
Homeostasis is the property of a system within the body of a living organism in which a variable, such as the concentration of a substance in solution, is actively regulated to remain very nearly constant. The word originates from two words: homeo and stasis. In the Greek language, homoios means similar and stasis means standing still. Thus, the word indicates “staying the same”. In the human body, there are internal and external variables operating at various points in time. In spite of such variables, the body maintains a fairly constant environment due to mechanisms of homeostasis.
The concept of homeostasis was first described by French physiologist Claude Bernard in 1865 and the word homeostasis was coined by American physiologist Walter Cannon in 1926. Canon postulated that homeostasis was a process of synchronized adjustments in the internal environment resulting in the maintenance of specific physiological variables within defined parameters; and that these parameters included blood pressure, temperature, pH, and others; all with clearly defined normal ranges. Canon further postulated that threats to homeostasis might originate from the external environment like extremes temperature or internal environment like an infection. The threats can be physical, psychological, or even emotional. Canon’s work outlined that the maintenance of the internal physical and psychological balance, homeostasis, demands an internal network of communication, with sensors capable of identifying deviations from the acceptable ranges and effectors to return these deviations back within acceptable limits. He identified negative feedback systems and emphasized that the response to variables within the body would be the same.
The metabolic process of all living organisms can only take place in very specific physical and chemical environments. The best-known homeostasis in the human body is related to maintaining temperature, pH, osmolarity, and concentrations of sodium, potassium, calcium, glucose, carbon dioxide, and oxygen. Take the case of body temperature. Core body temperature is regulated by a homeostat, with sensors in the hypothalamus of the brain. The setpoint of the regulator is regularly reset. Body temperature in humans follows a circadian rhythm, with the lowest temperatures occurring at night, and the highest in the afternoons. The temperature is 36.4°C from 2 a.m. to 6 a.m. and 37.5°C from 10 a.m. to 6 p.m. The regulator’s set point is readjusted in adult women at the beginning of a luteal phase of the menstrual cycle. The setpoint is again reset during infections to produce a fever.
Homeostasis does not govern every activity in the body. Take the case of blood pressure in mammals. It is homeostatically controlled and measured by stretch receptors in the walls of the aortic arch and carotid sinuses. The sensors send messages via sensory nerves to the medulla oblongata of the brain indicating variation in blood pressure. Subsequently, the medulla oblongata sends messages through motor or efferent nerves to a variety of effector organs. One of the effector organs is the heart. Stimulation of heart rate leads to tachycardia while lowering of heart rate is called bradycardia. Tachycardia or bradycardia may be set in when the blood pressure deviates below or above-set points of 80-120 mm of mercury. Thus, the heart rate for which there is no sensor in the body is not homeostatically controlled; however, it is one of the effector responses to errors in arterial blood pressure. Another example is of the rate of sweating. We sweat more in summer to maintain body temperature. Unlike this, we do not sweat in winter. We wear warm clothing to maintain body temperature. Apart from the entities which are homeostatically controlled in the internal environment of the body, some variables are neither homeostatically controlled nor involved in the operation of homeostasis. The blood urea concentration is an example. There are no sensors for urea. The blood urea is generated in the liver during the metabolism of amino acids of proteins. It is excreted by kidneys without active resorption or excretion by renal tubules. A high protein diet produces a high blood urea concentration. A poor protein diet with low blood plasma urea concentration leads to no secretion of urea in urine.
Homeostatic Mechanisms
There are two kinds of feedback in a chain-like event in the human body. The mechanisms are called as negative feedback and positive feedback respectively. Take a case of a chain reaction in which A is converted to B; B is converted to C; C to D and D to E. Quite often every change is controlled by the activity of an enzyme. The rate of every enzymatic reaction can vary. The slowest reaction is termed the rate-limiting step. If any of the intermediate from A to E is overproduced, a then higher concentration of the intermediate slows down the reaction leading to its generation. This is termed as negative feedback. Thus, negative feedback limits the higher production of an intermediate through a self-controlling mechanism. Alternatively, if the production of an intermediate is reduced below certain limits then related enzymes may be activated to restore the level of the intermediate. This is called a positive feedback mechanism.
Control of arterial pressure involves pressure monitoring system, volume monitoring system, hormonal mechanisms, reflex regulation, autonomic control, etc. Bradycardia due to higher blood pressure is an example of a negative feedback mechanism. In a cascade of reactions in coagulation, activation of one clotting factor leading to activation of other factors promoting coagulation to limit blood loss is an example of a positive feedback mechanism.
Operation of the feedback mechanisms involves three components:
- The sensor
- The control center
- The effector
The sensor contains receptors that monitor the change of the variable and provide the sensory signal to the controlling center as soon as the change is detected. The carotid sinus and the aortic arch contain baroreceptors in their valve to detect changes in blood pressure. They send signals to the controlling center located in the medullary oblongata.
The control centers are usually located in CNS( Central nervous system). Centers for blood pressure regulation are located in the medulla oblongata and hypothalamus.
The effector is the target organ which carries out the demand of the control center to achieve an effective response. Blood vessels and the heart are the effector organs related to blood pressure. Through bradycardia or tachycardia at heart and through vasodilation or vasoconstriction, they help in maintaining blood pressure.
Following control systems are important for the regulation of the human body:
- Core body temperature
- Blood glucose
- Plasma ionized calcium
- Blood partial pressure of oxygen and carbon dioxide
- Blood oxygen content
- Arterial blood pressure
- Extracellular sodium concentration
- Extracellular potassium concentration
- The volume of body water
- Extracellular fluid pH
As an illustration homeostasis of one parameter i.e. volume of body water is discussed below.
Homeostasis of Volume of Body Water
The volume of water in the body is measured by stretch receptors in the atria of the heart. They are also indirectly sensed by measurement of the osmolality of plasma by the hypothalamus. Measurement of the plasma osmolality gives an indication of the water content of the body. It relies on the fact that water losses from the body through sweat, gut fluids in the form of fecal water, and through vomiting/diarrhea and the exhaled air, are all hypotonic. It means that fluids like saliva, tears are less salty than plasma. Tears have almost the same salt content as that of extracellular fluids while saliva is hypotonic with respect to plasma. Thus, the taste of saliva is not salty while tears are decidedly salty. Nearly all normal and abnormal losses of body water make extracellular fluids hyper-osmolar. Conversely, excessive water intake dilutes the extracellular fluids making it hypo-osmolar. Only after loss of water through urine body can become isotonic. Hence excessive water intake leads to frequent urination.
When the hypothalamus detects a hyper-osmolar extracellular environment, it causes secretion of the hormone called antidiuretic hormone (ADH). For ADH, the kidney is the effector organ. The effect of ADH on kidney tubules leads to reabsorption of water from distal convoluted tubules and collecting ducts, thus preventing further water loss. Simultaneously, the hypothalamus stimulates the thirst center in the brain to stimulate the urge of drinking water. The cessation of urine flow prevents hypovolemia and hypertonicity from getting worse. Thus, drinking water corrects the defect.
Hypo-osmolarity leads to very low plasma ADH levels. This results in inhibition of water reabsorption from kidney tubules, causing high volumes of very to dilute urine to be excreted, thus getting rid of excess water in the body.
It is to be noted that urinary water loss, when the body water homeostat is intact, is a compensatory water loss, correcting excess of water in the body. Alternatively thirst reflex is an important second effector mechanism of the body’s water homeostat, correcting any water deficit in the body.
Stretching of the right atrium of the heart is a sign of excessive blood volume. It causes stretch receptors to secrete a hormone called an atrial natriuretic peptide (ANP) into the blood. It causes kidneys to get rid of sodium along with water loss into the urine. The net result is reducing the volume of circulating blood.
Thus, hypervolemia/hypovolemia is corrected by hormones like ADH / ANP. Water intake through the thirst center or urination by the kidney leads to the homeostasis of the volume of body water.
Homeostatic Breakdown
Many diseases are the result of the failure of one or more homeostat(s) in the body. The body water homeostat can be disrupted by the inability to secrete ADH in response to even the normal body water losses via the exhaled air, feces, and sweating. On not receiving ADH signals, the kidneys produce huge unchanging volumes of very dilute urine, causing dehydration and even death.
Another example is the type I diabetes mellitus. In this case, blood glucose homeostat ceases to function due to the destruction of beta cells of the pancreas. This means that the glucose sensor is absent and the effector pathway of insulin level in blood remains unchanged. The blood glucose concentration rises to very high levels, while the body’s proteins are degraded into amino acids and are used for generating energy via gluconeogenesis. If untreated, the condition can be fatal.
Make sure you also check our other amazing Article on: Female Reproductive System