Table of Contents
Heat Sterilization
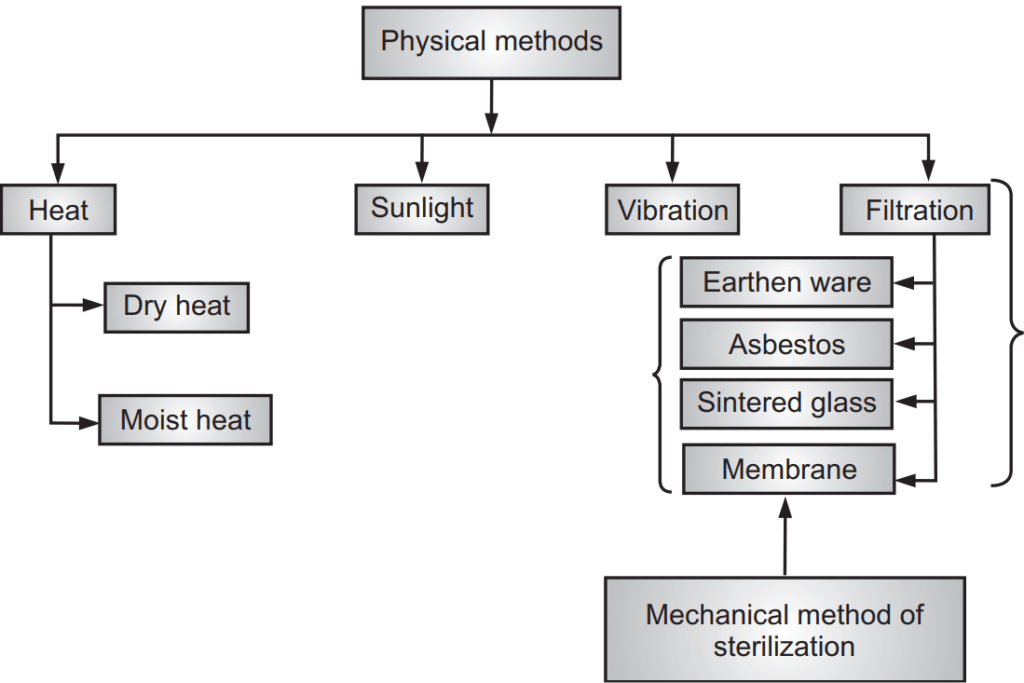
Heat is considered as the most reliable method of sterilization of objects that can withstand heat. It is carried out in two ways viz. Moist and Dry heat. They are the most common sterilizing methods used in hospitals and are indicated for most materials. This method of sterilization is applied only to the thermostable products, but it can be used for moisture-sensitive materials for which dry heat (160-180°C) sterilization, and for moisture-resistant materials for which moist heat (121-134°C) sterilization is used.
Advantages of Heat sterilization
- The most common method for controlling microbial growth.
- Very effective in destroying unwanted microbes.
- Low cost.
Disadvantages of Heat sterilization
- It is probabilistic i.e., not absolute sterilization.
- It can degrade thermally unstable media.
Dry Heat sterilization Method
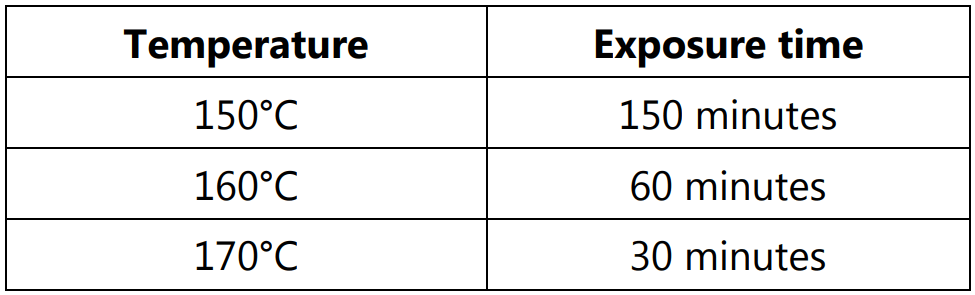
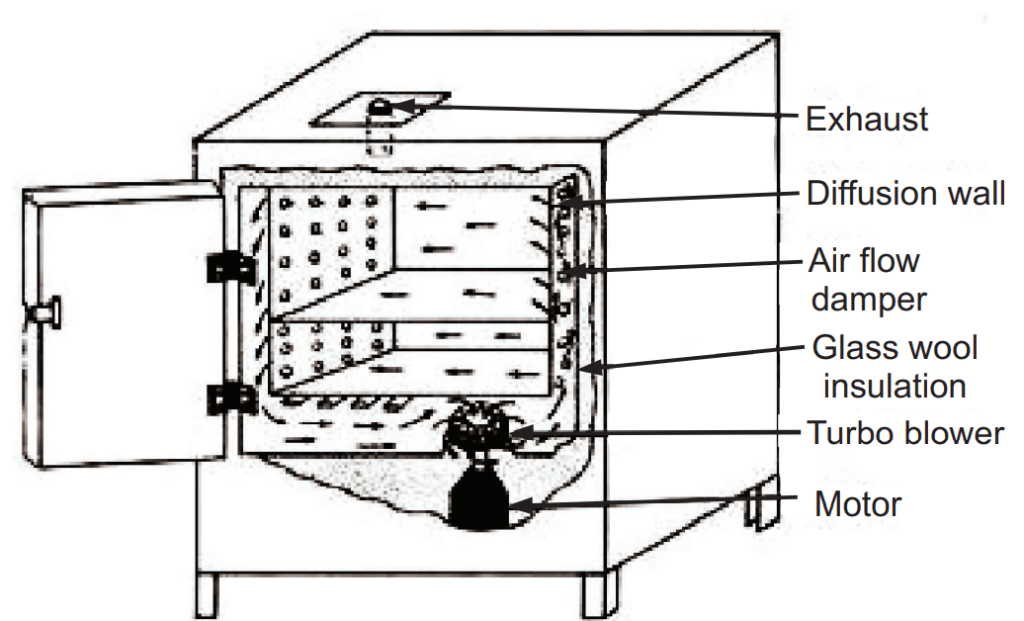
Dry heat sterilization requires higher temperatures and longer exposure times than moist heat sterilization. It uses high temperatures to kill microorganisms and bacterial spores and is used on items that cannot get wet and for glassware, oils, powders, metal instruments, and items wrapped in paper. There are three types of temperatures are recommended viz.
Thermal death time (TDT): It is the minimum time required to kill a suspension of the organism at a predetermined temperature in a specified environment. Thermal death time is inversely proportional to temperature. It is increased in presence of the organic substances, proteins, nucleic acid, starch gelatin, etc.
Principle: It causes denaturation of proteins and oxidative damage. There are several different types of dry heat sterilization such as:
- Red Heat: It is used for straight wires, bacterial loops, and spatulas.
- Flaming: It is the process of heating over the fire till they become red hot. It is used for bacterial loops, wires, and spatulas.
- Incineration: It is the process that involves the combustion of organic substances contained in waste materials. It is used for soil dressing, pathological bedding.
- Hot Air oven: It is an electrical device. The oven uses dry heat to sterilize articles at 50 to 300°C. The thermostat is used to control the temperature. It is commonly used in the dairy industry. Glasswares, forceps, scissors, scalpels, etc. are sterilized by this method but surgical dressings, rubber items, or plastic materials are not sterilized by this method.
The temperature used in a hot air oven with the holding time of articles is described as 160°C for 45 minutes, 170°C for 18 minutes, 180°C for 7.5 minutes, etc.
Operation:
- Articles to be sterilized are first wrapped or enclosed in containers of cardboard, paper, or aluminum.
- Then, the materials are arranged to ensure uninterrupted airflow.
- The oven may be pre-heated for materials with poor heat conductivity.
- The temperature is allowed to fall to 40°C, prior to removal of sterilized material.
Types of Hot Air Oven:
There are two types of hot air ovens.
(i) Forced air hot air oven and
(ii) Static air hot air oven.
The forced air hot air oven is more effective than the static air hot air oven. Forced hot air oven works by heating the oven and using a fan to move the hot air around whereas the static air hot air oven works by using a heating coil at the bottom of the oven. The heat rises throughout the oven and takes a longer time to reach the desired temperature.
Advantages of Hot Air Oven
Several advantages include:
- It does not cause metals to corrode or rust.
- It is relatively inexpensive.
- It does not release any harmful or hazardous fumes or pollutants.
Disadvantages of Hot Air Oven
- It is relatively slow (can take a couple of hours).
- Many objects cannot withstand the very high temperatures required for dry heat sterilization (for example some plastics would melt).
Applications of Dry Heat Sterilization:
The method is applicable for thermostable, moisture-sensitive pharmaceutical and medical devices and materials such as dry powdered drugs, suspension of drugs in non-aqueous solvents, oils, fats, waxes, oily injections, implants, ophthalmic ointments, etc.
Moist Heat
Principle: Moist heat is more efficient for sterilization in contrast to dry heat; it destroys microorganisms by the irreversible denaturation of enzymes and structural proteins. The temperature at which denaturation occurs varies inversely with the amount of water present.
Moist heat sterilization involves the use of steam in the range of 121-134°C. Steam under pressure is used to generate the high temperature needed for sterilization. Saturated steam acts as an effective sterilizing agent. There are three types of temperatures are used in this technique.
At temperature below 100°C:
- Pasteurization: Food industry.
- Vaccine bath: Vaccine sterilization.
- Serum bath: Serum contaminants, do not kill spores survive.
- Inspissation: Egg and serum-containing media, can kill spores.
At temperature 100°C:
- Boiling: Boiling water (100°C).
- Tyndallization (100°C).
At temperature above 100°C:
- Autoclave.
Pasteurization: This process was first discovered by Louis Pasteur. It is the process of heating liquids for the purpose of destroying viruses and harmful organisms such as bacteria, protozoa, molds, etc. This method is not intended to kill all microorganisms in the food. Instead, it aims to achieve a logarithmic reduction in the number of viable organisms, reducing their number so they are unlikely to cause disease.
Process:
- It involves milk.
- In the Holder method, the sample is heated for 30 minutes at 60°C.
- In the Flash method, the sample is heated for 15-20 sec at 72°C.
- Milk is not heated more than this temperature otherwise it forms aggregate resulting in the spoiling of milk.
- By this method, all non-sporing bacteria like mycobacteria, Brucellae, and salmonellae are destroyed.
- Coxiella burnetii being heat resistant survive Holder’s method.
Examples:
- Vaccines of non-sporing bacteria are pasteurized in the special bath at 60°C for 1 hour.
- A temperature of 80°C for 5-10 minutes destroys all vegetative forms of Bacteria, yeast, and molds.
- Spores of Clostridium botulinum are destroyed at 120°C for 4 minutes.
Inspissator: It is a system designed to produce large batches of uniform culture medium (Tuberculum bacteria culture) four to six times per day. Inspissation takes 50 minutes at 85°C. It is used for the sterilization of media.
Example: Lowenstein-Jenson and Loeffler were rendered sterile at 80-85°C for 30 minutes on three successive days inspector.
Boiling: It is the process of heating the sample to be sterilized material in a liquid at its boiling point to kill bacteria and other microorganisms and also spores.
Example: Vegetative bacteria are killed immediately at 90-100°C.
Steam at 100°C:
It is an inexpensive method of utilizing free steam to sterilize the culture medium. In this method, the container and the medium are simultaneously sterilized.
Tyndallization: It is also known as intermittent sterilization. It helps first exposure to kill all bacteria and spores. It is used for media with sugar or gelatin which requires 100°C for 20 minutes on three successive days.
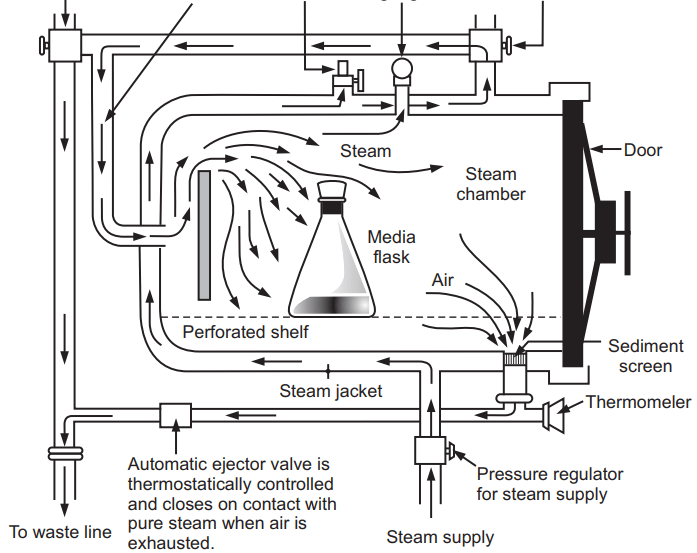
Autoclave:
It is also known as steam under pressure.
Principle:
High-pressure steam sterilization is used to kill all microorganisms, including spores. It is the best and most widely used method of sterilization. Example: Pressure cooker.
Vapour pressure within the autoclave increases that enabling steam to reach higher temperatures. At 103.4 kPa vapor pressure, the temperature reaches 121.3°C, for 15 ~ 20 minutes. This method is used for physiological saline, surgical instruments, containers, glass syringes, dressings, and another article (Fig. 1.2).
Autoclaves have lower row pressure pre-vacuum steam sterilizers which are classified into two types viz. portable and horizontal.
- Under the exhaust pressure steam sterilizer: With the upper part of the vessel, vapor pressure forces the cold air from the bottom of the exhaust vent. When the pressure in the 102.97 ~ 137.30 kPa, the temperature can reach 121 ~ 126°C, 15 ~ 30 minutes to achieve sterilization purposes.
- Pre-vacuum steam sterilizer: With vacuum before injecting steam into the first internal evacuated, a negative pressure is generated to facilitate steam penetration. When the pressure reaches 105.95 kPa, the temperature of 132°C, 4 ~ 5 minutes are enough for sterilization.
Advantages of Autoclave:
- It is rapid and effective.
- It destroys microorganisms more efficiently than dry heat and therefore a shorter exposure at a lower temperature is possible.
- It can be used for a large proportion of the official injections.
- It is supplied with dry saturated steam porous materials and can be sterilized without damage.
- Equipment or components of rubber and certain plastics such as nylon and P.V.C will withstand the conditions.
Disadvantages of Autoclave:
- Items sensitive to heat cannot be sterilized.
- It is unsuitable for anhydrous materials such as powders and oils.
- It cannot be used for injections and articles such as plastics that deteriorate at 115°C.
Advantages of Moist Heat:
- It has good penetration.
- It maintains the integrity of liquids due to the 100% humidity within the chamber.
Disadvantages of Moist Heat:
- Non-stainless steel metal items corrode in moist heat.
- It may damage rubber and plastic items.
- This method is not suitable for oils, fats, ointments, oily injections, etc.
Applications of Moist Heat Sterilization:
- This method is a most essential biocidal agent. It is used for surgical dressings, sheets, surgical and diagnostic equipment, containers, closures, aqueous injections, ophthalmic preparations, etc.
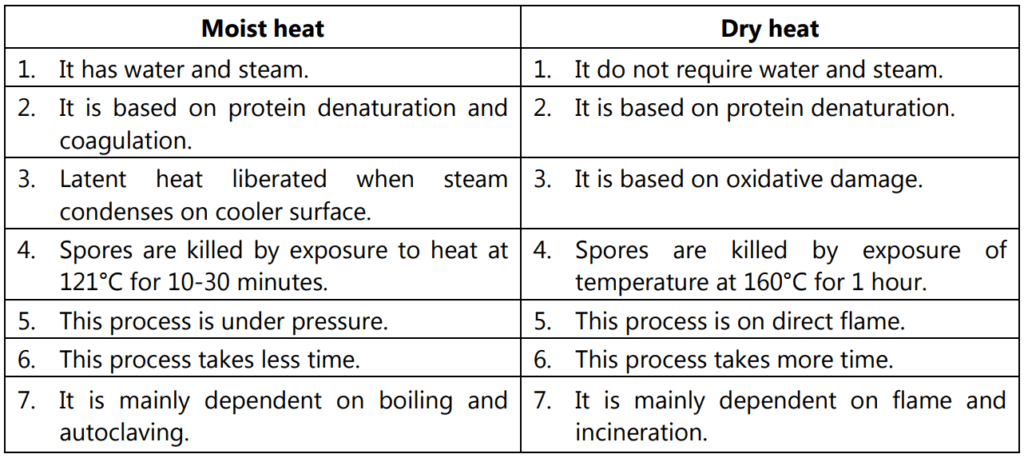
There are some differences between dry heat and moist heat sterilization (Table 1.1).
Sunlight:
It possesses bacterial activity. The action is due to its content of UV rays. Direct sunlight has a powerful germicidal action. Exposure to direct sunlight for a sufficient time will kill spores as well as vegetative cells. Tuberculosis germs are killed in a few hours. UV rays destroy bacteria in a few seconds or minutes; molds and yeasts are somewhat more resistant. Ultraviolet light is also used for the purification of drinking water and swimming pool water.
Ultrasonic Vibration:
It is the sound waves above the frequencies. Vibrations have the property to disrupt the cells. Gram-negative rods are more sensitive to ultrasonic vibration whereas Gram-positive cocci, spores of fungi, and resistant to the vibration. The current trend is to use ultrasonic as a cleaning agent to follow the process of sterilization in an autoclave.
Make sure you also check our other amazing Article on : Sterilization Process
