There are many subgroups in the genus mycobacterium such as M aviumintracellulare, M kansasii, M bovis, but M tuberculosis alone is pathogenic in humans. Mycobacterium tuberculosis most commonly affects the lungs. It is transmitted from person to person via droplets from the throat and lungs of people with active respiratory disease. Most commonly, tuberculosis is caused by air-borne infection.
In healthy people, infection with Mycobacterium tuberculosis often causes no symptoms, since the person’s immune system acts to “wall off” the bacteria. Most people who are exposed to TB never develop symptoms because the bacteria can live in an inactive form in the body. But if the immune system weakens, such as in immunocompromised (HIV) or elderly adults, TB bacteria can become active and their active state causes the death of tissue in the organs they infect. Active TB disease can be fatal if left untreated.
Tuberculosis is a communicable infection of lung tissue (pulmonary TB), and potentially other tissues (extrapulmonary or miliary TB).
Epidemiology
Tuberculosis is the most prevalent infectious disease in the world.
Tuberculosis is one of India’s major public health problems. According to WHO estimates, India has the world’s largest tuberculosis epidemic and approximately two to three million people are infected with tuberculosis out of a global incidence of 8.7 million cases. This is a public health problem. India bears a disproportionately large burden of the world’s tuberculosis rates, as it resides to be the biggest health problem in India.
Table of Contents
Causes
Tuberculosis is caused by Mycobacterium tuberculosis, which spread from person to person through microscopic droplets released into the air. This can happen when someone with the untreated, active form of tuberculosis, coughs, speaks, sneezes, spits, laughs, or sings.
Risk Factor
The person more prone to the infection includes:
- Immigration and infection with HIV
- Frequent and prolonged contact
- Host debilitation due to malnutrition enhances the risk of transmission (conditions exist in refugees living in poverty).
- Opportunistic infection (immunocompromised)
- Other risk factors include old age, alcoholism, diabetes, and environmental lungs disease.
Pathophysiology
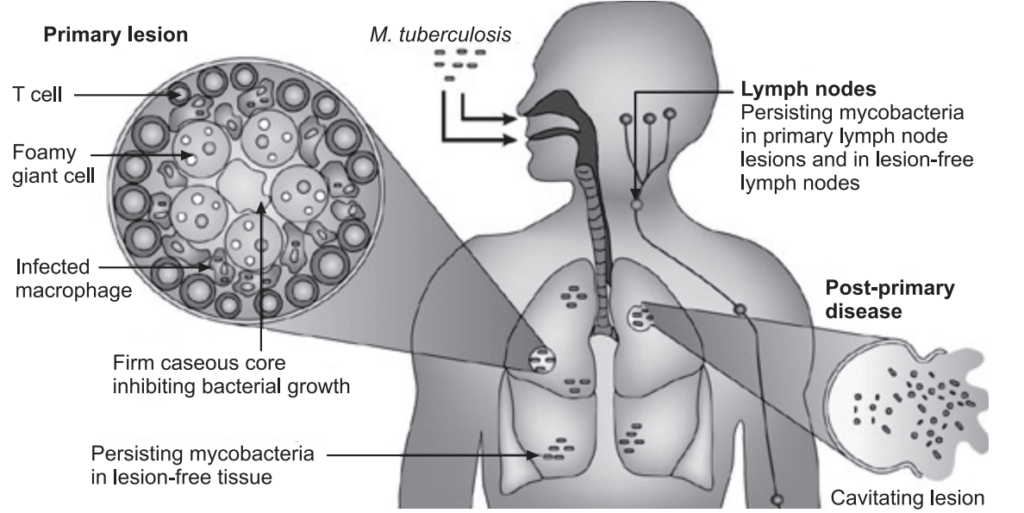
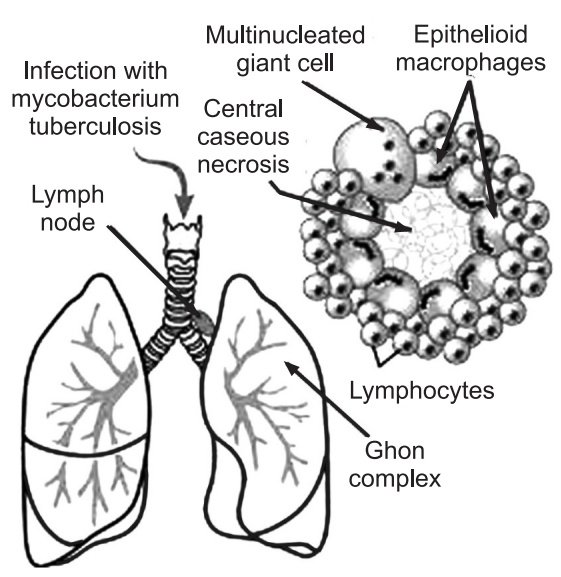
Infection with TB requires inhalation of droplet nuclei. Following deposition in the alveoli, Mycobacterium tuberculosis is engulfed by alveolar macrophages but survives and multiplies within the macrophages. Proliferating bacilli kill macrophages and are released; this event produces a response from the immune system. Exposure may lead to clearance of Mycobacterium tuberculosis, persistent latent infection, or progression to the primary disease. Successful containment of TB is dependent on the cellular immune system, mediated primarily through T-helper cells (TH1 response). T cells and macrophages from a granuloma with a center that contains necrotic material (caseous center,). Mycobacterium tuberculosis and peripheral granulation tissue consist primarily of macrophages and lymphocytes; the granuloma serves to prevent further growth and spread of M.tuberculosis. These individuals are non-infectious and have latent TB infection; the majority of these patients will have a normal chest X-ray (CXR) and be tuberculin skin test (TST) positive. Active TB typically occurs through a process of reactivation.
Approximately 10% of individuals with the latent infection will progress to active disease over their lifetime. The risk is greatest within the two years following the initial acquisition of M. tuberculosis. A number of conditions can alter this risk, particularly HIV infection, in which the annual risk of developing active TB is 8% to 10%. Immunocompromised conditions and treatment with immunosuppressing medicines, including systemic corticosteroids and TNF-α antagonists, also contribute to re-activation.
Clinical Manifestations
During initial infection and granulomas, there are no symptoms of mild bronchial pneumonia but the sputum test is positive.
Inactive TB, a sign of chronic inflammation includes:
- Anorexia,
- The overall sensation of feeling unwell,
- Weight loss,
- Fatigue,
- Low-grade fever,
- Night sweating,
- Coughing that lasts longer than 2 weeks with green, yellow, or bloody sputum,
- Shortness of breath,
- Chest pain,
- Hemoptysis.
The occurrence of additional symptoms depends on where the disease has spread beyond the chest and lungs. For example, if TB spreads to the lymph nodes, it can cause swollen glands at the sides of the neck or under the arms.
When TB spreads to the bones and joints, it can cause pain and swelling of the knee or hip.
Genitourinary TB can cause pain in the flank with frequent urination, pain or discomfort during urination, and blood in the urine.
Diagnosis
Medical history and physical exam include checking the symptoms such as an ongoing cough, fatigue, fever, loss of weight, anorexia, and night sweats.
Lab Tests include:
Sputum culture: Testing mucus from the lungs is used to diagnose active TB. But a sputum culture can take 1 to 8 weeks to provide results.
Sputum cytology: Examination of a sample of sputum (mucus) under a microscope to determine whether abnormal cells are present. It may be done to help detect certain non-cancerous lung conditions, such as pneumonia or inflammatory diseases, or the buildup of asbestos fibers in the lungs.
Test for TB Infection: The Mantoux tuberculin skin test (TST) or the TB blood test can be used to test for M. tuberculosis infection.
Additional tests are required to confirm TB disease. The Mantoux tuberculin skin test is performed by injecting a small amount of fluid called tuberculin into the skin in the lower part of the arm. The test is read within 48 to 72 hours by a trained health care worker, who looks for a reaction on the arm.
The TB blood test measures the patient’s immune system reaction to M. tuberculosis.
An uncertain reaction to the tuberculin skin test because of a weakened immune system, or to a previous Bacillus Calmette-Guerin (BCG) vaccination.
Chest X-ray: A posterior-anterior chest radiograph is used to detect chest abnormalities. Lesions may appear anywhere in the lungs and may differ in size, shape, density, and cavitation. These abnormalities may suggest TB, but cannot be used to definitively diagnose TB. However, a chest radiograph may be used to rule out the possibility of pulmonary TB in a person who has had a positive reaction to a TST or TB blood test and has no symptoms of the disease.
Rapid sputum test: This test can provide results within 24 hours. This test is done only when a person is strongly suspected of having TB.
Diagnosing TB outside the lungs: Diagnosing TB in other parts of the body (extrapulmonary TB) requires more testing. It includes:
Biopsy: A sample of the affected area is taken out to look for TB-causing bacteria.
Urine culture: This test looks for TB infection in the kidneys (renal TB).
Lumbar puncture: A sample of the fluid around the spine is taken to look for a TB infection in the brain (TB meningitis).
CT scan: This test is used to diagnose TB that has spread throughout the body (miliary TB) and to detect lung cavities caused by TB.
MRI scan: This test looks for TB in the brain or the spine.
Testing for HIV infection and blood test for hepatitis is often done at the time of TB diagnosis.
Tests during TB Treatment:
Drug Resistance: For all patients, the initial M. tuberculosis isolate should be tested for drug resistance. It is crucial to identify drug resistance as early as possible to ensure effective treatment. Drug susceptibility patterns should be repeated for patients who do not respond adequately to treatment or who have positive culture results despite 3 months of therapy.
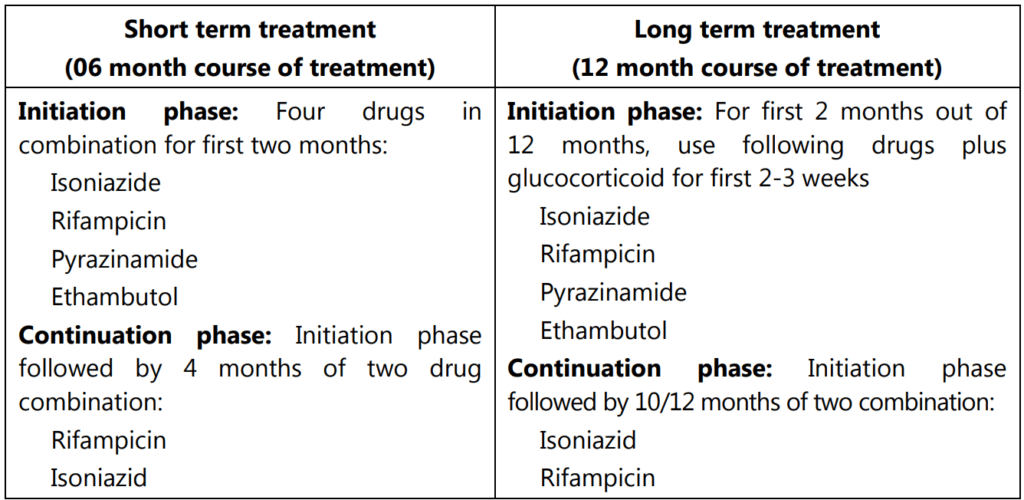
Treatment
Treatment for TB depends on whether it is active or latent. The patient may be hospitalized or suggested to avoid contact with other people until tests show that the patient is not contagious.
Antibiotics: For TB lung infections, antituberculosis drugs eg. isoniazid, rifampicin, ethambutol, Pyrazinamide, and streptomycin (Ist line) drugs are more effective. While para-aminosalicylic acid, thiacetazone, ethionamide, cycloserine, kanamycin, and rifabutin are IInd line drugs. A number of new drugs are available to overcome the current drug-resistant combination treatment including bedaquiline, delamanid, linezolid, and sutezolid.
If a particular type of TB infection is resistant to regular antibiotic treatment (a condition known as multidrug-resistant TB or MDRTB), a combination of different medications must be taken for 18 to 24 months.
Vaccination: A vaccine is available to limit the spread of bacteria after TB infection: The vaccine is generally used in countries or communities where the risk of TB infection is greater than 1% each year. It is used in newborns in these communities to prevent TB and its complications in the first few years of life.
DOT:
DOTS (directly observed treatment, short-course), is the name given to the World Health Organization’s recommended tuberculosis control strategy that combines five components:
- Government commitment (including both political will at all levels and establishing a centralized and prioritized system of TB monitoring, recording, and training).
- Case detection by sputum smears microscopy.
- Standardized treatment regimen directly observed by a healthcare worker or community health worker for at least the first two months.
- A regular drug supply.
- A standardized recording and reporting system that allows assessment of treatment results.
Clinical Features
- MTB has a remarkable tendency to develop resistance against antitubercular drugs. The drug treatment must be continued for many months, often a year or more. In the long period, the tubercule bacteria can become resistant to the drug even though the person is receiving antitubercular drugs. To prevent the development of resistance, one must use two or more drugs concurrently.
- Drug treatment consists of Ist line and IInd line drugs.
- Compliance: One major trouble is the noncompliance of the patient. This is a global phenomenon but is more common in poor countries. If compliance is good and the patient is immunocompetent, the cure rate is excellent, nearly 100%. Where compliance is defective recurrence rate is high.
- Host defense is also an important factor.
Prevention
Education and screening: To reduce the risk of infection and transmission, people with close contact with the patient may undergo prophylactic therapy. To minimize air-borne infection use protective measures such as covering the mouth and nose when coughing. Do not spend long periods of time in stuffy, enclosed rooms with anyone who has active TB until that person has been treated for at least 2 weeks. Someone who has active TB, help and encourage the person to follow treatment instructions.
Early diagnosis and treatment: TB should be treated early in order to prevent deterioration of the disease and the spread of the infection.
Leading a healthy lifestyle: The germs attack the lungs when a person’s body resistance is reduced. Try to guard by leading a healthy lifestyle in order to minimize the chance of contracting the illness. This includes adequate exercise, enough rest and sleep, a balanced diet, avoidance of smoking and alcohol, breathing fresh air, and maintaining good indoor ventilation.
BCG (Bacillus Calmette-Guerin) vaccination: The TB and Chest Service born babies to protect them against tuberculosis.
TB germs are spread by:
- TB germs are spread through the air when a person, who is sick with TB disease coughs, sings, sneezes, or laughs.
- To become infected with TB germs, a person usually needs to share air space with someone sick with TB disease (e.g., live, work, or play together).
- The amount of time, the environment, and how sick the person is all contributing to whether or not get infected.
- In most cases, the body is able to fight off the germs.
TB germs are not spread by:
- Through quick, casual contact, like passing someone on the street.
- By sharing utensils or food.
- By sharing cigarettes or drinking containers.
- By exchanging saliva or other body fluids.
- By shaking hands.
- Using public telephones.
Make sure you also check our other amazing Article on: Leprosy